The latest Nursing Council statistics for nurses seeking verification of their registration so they can practice in Australia show 1555 nurses applied in the year to March 31 2017 – more than double the rate of two years ago.
Since about 2006 the number of Kiwi nurses applying to nurse across the ditch had been steady at around 1200 to 1500 but had slumped to just 750 in the 2014-15 year and rose only slightly to 819 in 2015-16.
The 2017 statistics showed a steep increase in nurses seeking to nurses overseas in all destinations (up from 1272 in 2015-16 to 1804 in 2016-17) but has still not reached the peak years of 2001-02 and 2011-12 when more than 2200 nurses sort verification of their registration to work overseas.
How many of last year’s 1555 applicants were planning to permanently move to Australia in is unknown as a number of Kiwi nurses are known to cross backwards and forwards across the Tasman to take on lucrative short-term – mostly rural and remote – nursing contracts.
What is known from Nursing Council annual practising certificate (APC) stats is that in 2016 there were 1347 overseas-based nurses with valid New Zealand APCs. Which indicates that many nurses keep the option open of returning to nurse in New Zealand.
Outgoing Chief Nurse Dr Jane O’Malley said Kiwis would continue to go to Australia but what was most important was ensuring that new graduate nurses start their careers in New Zealand. “So when they finish in Australia they are more likely to come back and practice in New Zealand then if they had never practised here.”
She was particularly encouraged by the latest Ministry of Health and ACE analysis which indicated that 86 per cent (806) of the 2012 nurse graduates who gained a place in a government-subsidised NETP (Nurse Entry to Practice) programmes were still in nursing five years on – and only about a dozen of those were not practising in New Zealand. Overall more than 80 per cent of the 1514 new graduates registered in 2012 were still nursing in New Zealand five years after graduating.
]]>
This is a familiar path that thousands of Kiwi nurses have followed before her. In the ’50s they went by ship and in the ’70s many travelled overland via the hippy trail but the most common OE destination was the ‘mother country’, England, where New Zealand nurses could typically easily get nursing jobs, earn some money, travel and gain some experience in some of London’s top teaching hospitals at the same time.
But since 2005 registering as a nurse in the UK as a non-EU trained nurse has become increasingly more complex and expensive, resulting in Stanley being part of a new generation of Kiwi nurses on their UK OE who opt to put nursing aside for a while to work as live-in carers.
Stanley graduated in late 2014 from the University of Auckland nursing school and went to work in the surgical ward of a private hospital. With two years’ experience under her belt she decided to follow her sister and some non-nursing mates and head off.
Initially she planned to just be away for six months so didn’t think the complex and costly UK RN registration process was worth pursuing, and having heard about live-in care work she decided it sounded a much simpler option. She has now stretched her OE plans to closer to 15 months – long enough away to see a good chunk of the world but not too long from nursing to put her annual practising certificate (APC) in jeopardy.
Stanley is in the UK on a Youth Mobility Scheme (YMS) visa that allows 18–30-year-olds from New Zealand (and seven other eligible countries) to work in the UK for up to two years.
She is based in Oxford, working for agency Oxford Aunts as a level-four carer working with complex clients needing advanced-level carers. Her first client was for just a month and she has been with her second, who requires a hoist to get in and out of bed, since August.
“The downside of live-in care obviously is that you do sacrifice a bit of your social life but it is really worth it for the experience of giving one-on-one care to a person. You can really make a positive difference to their life.”
The sacrifice is rewarded by free board and food, a combination that has allowed her to save funds to travel around Europe and Asia with mates, plus have the security of slipping back into the same job on her return to UK as a reliever steps in to look after her long-term client while she takes leave.
In September she went to France, Italy and Germany for about a month; in November she spent two weeks in Europe; and she has recently returned from India and Sri Lanka and another trip to France.
Stanley says her actual hourly pay rate is similar to what she received as an RN for less stressful work, but she works more hours. Typically her contract is for 8–10 hours’ work a day – spread across the day for when her client needs her – but she has a three-hour break outside the house once a day, and once a week a reliever provides an eight-hour break, during which she can visit friends in London or head elsewhere on a day trip.
Stanley is planning to return in home in July. She says she is not tempted to stay on and seek registration, even though there appear to be nursing jobs available from what she saw online.
“The trouble is that the pay of nursing jobs is not very good in the UK – I think it’s almost worse than New Zealand from my limited research. Also if you are going to live in London to nurse, the cost of living is insane.”
For now she is planning to return to work in a surgical or medical setting to broaden her nursing skills. But she says her time as a live-in carer has made her passionate about aged care and sparked her interest in working in this area in the future. But first she has one final big trip to do before she finishes her OE and heads back downunder to resume her nursing career.
]]>This backs ongoing calls by the national nursing organisations for 100 per cent placement of new graduates in new graduate programmes – a goal they had set to be met by this year.
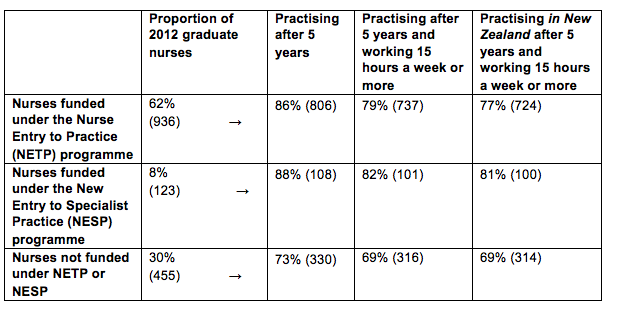
The Ministry of Health analysis found that 86 per cent (806) of the 2012 nurse graduates who gained a place in a government-subsidised NETP (Nurse Entry to Practice) programmes were still in nursing five years on.
The proportion was even higher for mental health nurses with 88 per cent of the 123 new grads signed up to a specialist mental health NESP (New Entry to Specialist Practice) Programme) still having valid annual practising certificates (APC) five years later.
In comparison just 73 per cent (330) of the 455 new graduates who failed to gain a place in a NETP or NESP programme still had an APC in 2017. Overall 1244 (82%) of the 1514 nurse graduates registered in 2012 were still in nursing five years later. (See table below)
Chief Nurse Jane O’Malley said the higher proportion of new graduates still nursing if they had started their careers in a funded new graduate programme was “telling” and showed the importance of the programmes for nursing retention.
In 2013 the National Nursing Organisations – including the New Zealand Nurses Organisation and College of Nurses Aotearoa – called for full utilisation of all NETP funding to support the goal of 100 per cent employment of new graduates by 2018. Government funding is potentially available to subsidise 1300 NETP and about 125 NESP places but lack of vacancies and tight budgets – particularly at district health boards – means only all the NESP funding is fully utilised.
New graduate nurses employed under a year-long NETP programme must receive clinical preceptor support for the duration of the programme and the equivalent of 12 study days with the aim of new nurses starting their career “well supported, safe, skilled and confident in their clinical practice”.
The analysis of the 2012 new graduate cohort – that uses data from the ACE new graduate placement and Nursing Council of New Zealand annual practising certificate data – also showed the vast majority of the new nurses still holding APCs were practising for more than 15 hours a week. (NB nurses practising for less than 15 hours a week but still with valid APCs may be on parental leave, travelling overseas or between jobs.)
The APC data indicated that just over a dozen nurses with valid New Zealand APCs were currently practising overseas. (Retaining an NZ APC indicates that they may only be working overseas for a limited amount of time and/or wanted to retain the option of returning to New Zealand to nurse.)
]]>
The United States’ CDC (Centers for Disease Control and Prevention) reported late last week (Feb 8) that levels of influenza-like-illness (ILI) had reached the peak of the 2009 H1N1 pandemic with unusually high numbers of hospitalisations in the 50-65 age group.
CDC reported that it didn’t believe the flu season had peaked in the US yet but the United Kingdom’s Public Health Service at the same time reported that flu numbers had stabilised and at this stage didn’t seem as severe as some other recent seasons. Both countries reported that the main flu strains circulating were flu A(H3N2) plus H1N1 strains and flu B strains.
Last year 66 per cent of district health board employees received the influenza vaccine – up on 61 per cent in 2014. Doctors remain the profession with the highest uptake of the flu vaccine with 72 per cent receiving the jab last year but nurses are now not far behind having increased their uptake from 59 per cent in 2014 to 68 per cent last year.
The DHB with the highest nurse vaccination rate remained Tairawhiti at 84 per cent followed by Auckland, Northland and Waikato all at 81 per cent. The DHBs with the lowest nurse vaccination rates were Wairarapa (47%), Lakes (49%) and MidCentral (55%).
Midwives remain the profession with the lowest uptake which fell from a high of 59 per cent in 2015 to 54 per cent last flu season.
The Immunisation Advisory Committee (IMAC) and Ministry of Health are again pointing out that healthcare workers can transmit influenza without knowing they are infected as the flu doesn’t always cause symptoms or make people unwell.
Data from the Southern Hemisphere Influenza and Vaccine Effectiveness Research and Surveillance (SHIVERS) study, based in Auckland, suggest that four out of five children and adults (80%) with flu were asymptomatic. And an earlier study – following the 2009 ‘swine flu’ pandemic in New Zealand – found almost one quarter of the adults who reported that they had not had influenza in 2009 were tested and found to have been infected by the H1N1 virus that caused the pandemic.
The New Zealand-based Southern Hemisphere Influenza and Vaccine Effectiveness, Research and Surveillance (SHIVERS) study has indicated that flu vaccine effectiveness in New Zealand is around 50 per cent or more.
Four strain vaccine available this year
Pharmac has confirmed that this year it will be funding for the first time a flu vaccine targeted at four strains of the flu virus rather than the usual three strains.
Two forms of quadrivalent vaccine will be funded from March 1 with Influvac Tetra funded for eligible people aged three years and over and another vaccine, Fluarix Tetra, funded for eligible children aged 6 to 35 months.
Pharmac deputy medical director Dr Bryan Betty says the four-strain vaccine will offer additional protection against influenza in 2018, and into the future.
Pharmac negotiated long-term supply with Mylan in 2016, including provision for a four-strain vaccine once it was approved for use by Medsafe. This has now occurred.
The funded vaccines will both contain the strains of influenza virus specified by the World Health Organisation for the 2018 Southern Hemisphere influenza season which are:
- an A/Michigan/45/2015 (H1N1)pdm09-like virus;
- an A/Singapore/INFIMH-16-0019/2016 (H3N2)-like virus; and
- a B/Phuket/3073/2013-like virus
- a B/Brisbane/60/2008-like virus
CDC Acting Director Dr. Anne Schuchat said last week that it was known that flu vaccines can often have lower effectiveness against H3N2 viruses but added that “however some protection is better than none” against the virus strains which were often linked to more severe illness – especially among children and people aged 65 and older.
Stock of the New Zealand seasonal influenza vaccine is typically available from early March until 31 December each year.
The exact start date for the 2018 seasonal influenza vaccination programme will be notified by the Ministry of Health in due course. The Fluarix Tetra vaccine for children under 3 years is likely to be available from mid-April 2018.
7876IMAC 2017 FLU_infographic_audio from Theo Brandt on Vimeo.
]]>Applications opened today (February 14) for the scholarships that are open to Māori students in nine health disciplines including community health workers and health management.
Associate Minister of Health Jenny Salesa said the scholarships were a great opportunity for students and health care workers and offered them support to help them achieve and excel in their chosen health career. She also said enhancing and encouraging Māori representation in the health workforce is hugely important so that the system responds effectively to the needs of Māori.
Currently nurses identifying as Māori make up about seven per cent of the total nursing workforce while Māori comprise about 15 per cent of the New Zealand population. But the percentage of Māori nurses may be on the increase with Māori nurse graduates making up 14-15 per cent of applicants to the latest two rounds of the ACE new graduate job matching process.
There are 11 Hauora Māori scholarship categories (covering nine specific health disciplines plus other undergraduate health-related degrees and Māori students studying towards a postgraduate qualification). There are also three special award categories: the Excellence Awards, the John McLeod Award and Te Apa Māreikura Award. The scholarships and awards range in value from $1000 to $10,000 each. Nursing scholarships are worth $1700 each.
To be eligible for a Hauora Māori Scholarship, applicants must be a student enrolled and attending a university, polytechnic, wānanga or private training establishment based in New Zealand and have whakapapa and/or cultural links with Te Ao Māori or Māori communities.
They must demonstrate a commitment to and/or competence in Māori health and wellbeing and be studying a health or disability-related, NZQA accredited course.
Online applications open at 5pm today (14 February) and close on 28 March.
More details are available on the Ministry of Health website: http://www.health.govt.nz/our-work/populations/maori-health/hauora-maori-scholarships-2018
]]>
Waikato DHB’s acting chief executive Derek Wright has asked for a review of the previous CEO Nigel Murray’s policy of requiring non-vaccinated health workers to wear masks while delivering patient care.
Murray brought the unpopular VOM (vaccinate or mask) policy with him from his old employer, British Columbia’s Fraser Health Authority where the policy had successfully withstood a union legal challenge.
Waikato introduced the hardline policy in 2015 – including suspending two unvaccinated nurses – and saw its nurse vaccination rate jump from 52% in 2014 to 81% in 2015, 80 per cent in 2016 and 81 per cent again last year.
The New Zealand Nurses Organisation has been on the record that while the organisation was quite clear it encouraged nurses and other members to get the seasonal flu vaccine, it also had “significant concerns” about the co-ercive nature of a VOM policy.
Waikato’s staff immunisation rate has never surpassed Tairawhiti DHB whose positive campaign – centred around a focused week-long campaign into every DHB department followed by catch-up clinics near the staff cafeteria – has kept the DHB at the top of the vaccination tables for four years with 84 per cent of both nurses and overall staff getting the flu jab last season. Tairawhiti also had the highest percent of ‘other’ DHB staff getting immunised at 90 per cent and the highest percentage of midwives with 88 per cent.
A Waikato spokesperson said the DHB had decided it was timely to revisit the VOM policy to see whether it was working. “Our Infection Control Committee will be looking at the evidence and research around masking and make a recommendation to the Executive. It could mean the policy is amended, or it could remain,” said the spokesperson. She said Wright was keen to work with staff and find the best solution for the DHB’s staff which also kept patients safe. “Obviously getting immunised and staying home if you are sick is the best protection for everyone.”
The DHB’s acting chief executive initially trained as a general nurse and then mental health nurse in the United Kingdom and worked in a variety of mental health management positions in the UK, New Zealand and Australia before joining Waikato in early 2016 as the DHB’s mental health director.
]]>It warned that New Zealand was “quickly becoming a society divided by the ownership of housing and its related wealth”.
It also showed home ownership had slumped dramatically since the 1980s – especially among Pacific and Maori people – and Auckland’s housing problem was created by a mix of population growth, partly fuelled by migration, and the construction and land development sectors “hindering” housing affordability.
It also pointed to a potential time bomb in the impact on housing affordability on the elderly, finding the proportion of older people who were living in mortgage-free homes had dropped from 86 per cent to 72 per cent since the 1980s.
The housing report was authored by economist Shamubeel Eaqub, University of Otago Professor of Public Health Philippa Howden-Chapman and the Salvation Army’s Allan Johnson.
‘Sobering’ reading
Twyford said it was “sobering”.
“It paints a sobering picture of the devastating impacts of the housing crisis, particularly on children. Homelessness, transience and substandard housing have had a lasting and sometimes even deadly effect on our youngest.”
It included discussion of the “hidden homeless” population that is not officially monitored or recorded.
However, community emergency housing providers report they are at full capacity, and their data from last year indicates that for every 10 homeless people that approach them, eight to nine are turned away.
The report shows homelessness was worse than previously thought and that 80 per cent of homeless people turning up to community emergency housing providers in the last year were turned away.
It brings together figures across a number of areas including homelessness, the rental market, housing affordability – including the rising costs relative to wage increases – and housing supply nationwide, with a specific focus on Auckland.
The report warns of a burgeoning “floating population” – people without safe and secure housing, including in temporary housing, sharing with another household, or living in uninhabitable places.
Greater awareness of the issue, along with more information campaigns about where to get help, is expected to lead to reported homelessness getting worse.
The report is intended as analysis of the housing issue, and is not expected to make any recommendations for action.
One indication of the extent of the crisis in the report is an extra 2000 pensioners receiving the accommodation supplement last year.
‘Pipeline of homelessness’
Alan Johnson of the Salvation Army was one of the report’s authors. He warned that homelessness would get worse before it got better.
“We believe there’s a pipeline of homelessness still in existence. There will be some time yet before we see the numbers in transitional housing tapering off. We believe it will get worse before it gets better.”
He had looked at housing assistance programmes, homelessness and transitional housing. He said the previous National Government’s reforms in the area of social housing and state housing were “poorly funded and poorly executed”.
“It’s apparent to us that one of the problems we’re had in social housing or state housing areas was that the previous government’s reform agenda was in parts an essential programme in terms of rejuvenation of housing stock, but the reality is it was poorly funded and poorly executed.”
Johnson said reform of the Accommodation Supplement was needed, beyond the increase due mid-year under the Government’s families package as hundreds of thousands were dependent on it.
He said abatements created ”poverty traps” and the current system was arbitrary and could act as a disincentive for people to take on part-time work.
He said there should be a preference for fixed-term tenures, rather than periodic, and those should provide a way to moderate rent increases.
The Tenancy Tribunal was funded from the interest off tenants’ bonds, yet it was landlords who used the Tribunal more. That funding should be used more for tenants’ rights, he said.
Otago University Public Health professor Philippe Howden-Chapman said the numbers of children who did not live in homes owned by their families had grown.
“This has fundamentally major consequences for stability in communities.”
She said in Otago’s “Living in New Zealand” long-term study, those who had not lived in stable housing as a child had faced different consequences than others.
She said little work had been done on the social costs of substandard housing in New Zealand and it was beneficial for the government to be looking at the consequences of housing on the wellbeing of people.
Economist Shamubeel Eaqub has hit out at the Labour Government’s fiscal responsibility rules, saying it was acting as a “straitjacket” on it and debt could be used to reform the housing market.
Eaqub was one of the authors of a housing stocktake commissioned by the Government to help guide housing policy.
Eaqub said investment was needed in infrastructure and housing such as the KiwiBuild programme yet the Government was restricted because of the fiscal responsibility rules.
He said the infrastructure issue could be resolved by “borrowing s***loads of money” and only a “fiscal idiot” would not have been borrowing money in the current climate or over the past decade.
Labour and the Greens both signed up for fiscal responsibility rules requiring the Government to stay in surplus and to gradually reduce government debt relative to GDP to 20 per cent.
Housing report: key points
• Population has outstripped housing growth by 2.1 per cent
• New Zealand has 1.9 million private homes with average of 2.6 people per dwelling • 574,000 households are renting
• Rents for three-bedroom houses rose 25 per cent 2012-17, but wages just 14 per cent
• 32 per cent of rental properties are “poorly maintained”
• 29 per cent of households struggle to afford power bills, spent a large portion on the bill, or felt cold
• Number of children under 15 living in rentals up 65 per cent between 1986 and 2013
• Child asthma estimated to have cost $58.3m in 2013
• Between 1991 and 2013 the proportion of Maori renting privately rose from 41 per cent to 77 per cent and for Pasifika from 27 per cent to 56 per cent.
• “This rise appears to be fuelled by the decrease in state housing stock and changes to policies designed to move people out of state housing.”
• 6128 households needing a state house in December 2017
• One in 100 people homeless in 2017, up from one in 120 in 2006
• For every 10 people approaching emergency housing providers in 2017, eight or nine turned away
Source: A Stocktake of New Zealand’s Housing.
The interim chief executive at Waikato District Health Board has spent most of his career in health managing broken situations back to repair.
As the replacement for Dr Nigel Murray, who resigned in October amid an expenses scandal, Wright is arguably tasked with his biggest challenge yet.
That is; change the culture, create a workplace people are proud of, get Waikato Hospital to the top of its game, and turnaround the DHB’s financial problems.
The 63-year-old has set himself a one year deadline to achieve the transformation.
He doesn’t want to commit for too much longer than that for two reasons – he gets bored easily which turns to “mischief”, and he wants the next chief to hunker down for five years and lead the embattled DHB into a period of stability, security and ultimately, growth.
And it should be noted, Wright – previously the health board’s mental health and addictions executive director – was given the seal of approval for the important interim job by the senior doctors at Waikato Hospital.
This is no mean feat, particularly given the dysfunctional relationship Murray created with clinicians during his three year tenure, and the loss or partial loss of training accreditation in different units at the tertiary hospital.
Wright says there’s no secret to being a good leader.
“It’s not rocket science. I think it’s about having that focus, having that visibility. I’m really clear that I make decisions everyday that impact on the work that staff do and unless I’m informed then I might be making the wrong decisions.”
Relating to people from all walks of life comes naturally to Wright.
Born in Scotland and raised in Fife, north of Edinburgh, Wright fell into health at 19 when his neighbour offered him a job at the local hospital as an orderly.
“I started at the bottom basically.”
The football-mad teenager earned just 10 pounds per week, about $200 by today’s standards, graduating to 15 pounds a week after he trained to be a nurse.
That was 1978. He specialised in surgery and crossed into mental health, working his way up from a staff nurse to a charge nurse.
He moved to Newcastle in 1984 at the time when major health reforms were underway with an emphasis on turning clinicians into managers.
Wright was offered a spot at Birmingham University to study health management and moved into general management shortly after.
By then he was married to Elizabeth – who he met in the nurses’ home of a psychiatric hospital – and together with their two children in 1992 the couple upped-sticks and moved to New Zealand on a health industry exchange for one year.
Wright swapped jobs with the manager at Auckland mental health services based at Waitemata.
“During that year I also got asked if I would take on the role of project manager for the closure of Kingseat [Hospital] and Carrington [Hospital].
“I think it was because, ‘new guy, if it doesn’t work then he’s out of here and if it does then he’s out of here anyway and we can take the credit’.”
Wright closed the two former mental hospitals – Kingseat took longer than a year – and back in the UK he and Elizabeth decided, thanks to a bitterly cold winter, they would make New Zealand home permanently.
He managed mental health and drug and alcohol services at Waitemata from late 1993 before becoming general manager of North Shore Hospital for four years.
That was followed by a stint as the first mental health regional director for the northern region before Wright was headhunted in 2007 to be director of operations in South Australia.
“The day I arrived, they had 74 psychiatrists and 40 of them resigned. Nothing to do with me. It was all to do with pay negotiations they were having with the state but that was my introduction to South Australia.”
Five years later Wright returned to New Zealand. He worked for a non-government organisation and was made redundant.
He set up a consultancy, doing strategic planning, restructures and service reviews, including a mental health review for Northland.
Wright initially turned down the opportunity to apply for the mental health director role at Waikato, but eventually succumbed to a persistent recruitment agent.
He joined the DHB in February 2016, during the middle of a Ministry of Health Section 99 review of its mental health unit, following the death of patient Nicky Stevens.
Among other things, the review identified the need for an experienced senior executive in the DHB’s mental health team, a position left vacant during a restructure of the executive leadership by Murray.
The DHB had also been in the spotlight for allowing fake psychiatrist Mohamed Siddiqui to work there for six months in 2015 on a salary of $165,000.
“There was lots to do but there was a really good team and me never having worked in Waikato before, I came in with fresh eyes. We made lots of changes. There was already lots happening – I just hopefully provided some leadership to the team.”
Wright has already been outspoken on some issues. He previously said he believed New Zealand had too many district health boards.
Twenty for a population of 4.5 million is out of kilter he reckons, and he believes there should be one linked IT system for all DHBs so that health records follow patients.
He also wants to see real change come from the ministerial mental health inquiry launched last month, not just “a tinker and throwing money” at the problem because as it stands our mental health system is unsustainable, Wright says.
Plus there’s room for better training, Wright suggests. Much of his training was on the wards compared to today’s student nurses, some of whom get all the way through a nursing degree only to find the profession is not for them once they get properly into a hospital.
“I think the pendulum has gone too far. I think probably when we trained in the ’70s we were a cheap workforce. I think here there’s too much of the academic side of it and not enough of how do you deal with people.”
Nowadays Wright says there are lots of expectations from health that didn’t exist 40 years ago.
“In the early ’70s, if you were a patient and you needed a hip replacement and you were 65, you didn’t get it done.
“Whereas we operate on 90 year olds now because the expectation is you get it done.”
For now though Wright will concentrate on the job at hand – restoring public confidence in Waikato DHB.
He has set about doing this with a number of initiatives including recently proposing to trim his executive leadership team, to dismantle the 18-strong group Murray put in place and re-assemble it so only 11 executives report directly to him.
Wright also returned the executives to Waikato Hospital after Murray moved them to an ivory tower in the city, away from the coalface clinicians felt.
There’s a 10-year plan being developed focusing on prevention and working smarter, and staff at the $1.4 billion organisation have rallied behind it.
He’s confident of regaining the lost training accreditation in obstetrics and gynaecology and is working on creating a workplace free of bullying and where targets feel they can speak out.
Wright will continue visiting the DHB’s 7000 staff including those at hospitals in Taumarunui, Tokoroa, Te Kuiti and Thames, and he is tackling the way the DHB communicates, both internally and externally.
It’s undoubtedly damage control after the DHB was accused of keeping information secret during the Murray affair, but making himself available to the media and sending out fortnightly intranet updates to staff, complete with jokes, is a good start.
“I’ve hopefully brought some consistency to the organisation. I do a lot of management by walkabout. It’s a slightly different culture I’m trying to bring to the organisation. I guess I’m just trying to humanise management.”
]]>The link between unhappy patient and too few nurses per patient in England’s National Health Service (NHS) hospitals was found in a major quantitative study led by researcher Linda Aiken.
The study, published in the British Medical Journal earlier this year, is the first to bring together data on patient to RN staffing ratios, missed nursing care and patient satisfaction with NHS hospital care in England. Researchers say their findings refutes claims that quality of care deficits in NHS hospitals were due to uncaring nurses.
The study, led by Aiken, the professor of nursing at the University of Pennsylvania, said, highly publicised reports citing preventable deaths and deficiencies in hospital care in England, like in Mid-Staffordshire, had uniformly concluded that inadequate hospital professional nurse (RN) staffing was a contributing factor.
But she said that despite that leading to national guidance on safe staffing there was still substantial variation in staffing levels across NHS hospitals and the value of more RNs per patient was still questioned at the policy level.
Data gathered during the RN4CAST study found that nurse workloads averaged 8.6 patients per RN during the day, and ranged from 5.6 patients per RN to 11.5 patients per RN across the 46 hospitals involved in the English arm of the international research study.
“National survey data from patients experiencing a hospitalisation in an NHS hospital in England confirm that patients have a high level of trust and confidence in RNs.” The study said this evidence refuted the media reports blaming quality of care deficits in NHS hospitals on uncaring nurses.
“However, only 60% of patients indicated that there were always enough RNs to care for them, and 1 in 10 patients indicated that there were never rarely enough RNs. The importance to patients of adequate RN staffing is evident in their responses; 57% of patients who indicated that there were always or nearly always enough RNs to care for them rated care as excellent, compared with only 14% of the patients who said there were rarely or never enough.”
The researchers said additional analyses undertaken indicated that patients in hospitals with poorer RN staffing were much less likely to say there were always enough nurses to care for them.
“We estimate, from models that took account of numerous confounds, that the likelihood of patients saying there were always enough nurses to take care of them were about 40% lower in hospitals in which the average nurse took care of 10 patients than in hospitals in which the average nurse took care of 6 patients. These findings reinforce from patients’ perspectives the importance of adequate hospital RN staffing.”
The researchers concluded that the evidence showed that English patients expressed a high level of confidence and trust in nurses; and their satisfaction with hospital care was less favourable when they perceived there weren’t enough nurses available.
“The narrative that quality deficits in hospitals in England are due to ‘uncaring’ nurses is not supported by the evidence. On the contrary, our findings suggest that reducing missed nursing care by ensuring adequate numbers of RNs at the hospital bedside and improved hospital clinical care environments are promising strategies for enhancing patient satisfaction with care.”
The full study can be viewed at: http://bmjopen.bmj.com/content/bmjopen/8/1/e019189.full.pdf
]]>Dr Michal Boyd, an aged care NP and nurse leader who last week was celebrating at last being able to issue death certificates for her patients’ families said it was a “terrible blow” to discover that NPs were still blocked from signing cremation certificates.
More than a decade in the making, the Health Practitioners (Replacement of Statutory References to Medical Practitioners) Bill was passed in late 2016 but the changes made only come into effect on January 31.
The complex Bill amended eight Acts to replace references to ‘doctors’ or ‘medical practitioners’ where nurse practitioners (NPs), and other health practitioners like pharmacists, registered nurses and physiotherapists are now qualified to carry out those roles – but did not amend the related Cremation Regulations. This means cremation certificates still have to be signed by a medical practitioner, which is a particular frustration for NPs working in aged care.
Ministry of Health chief nursing officer Jane O’Malley said the Ministry was aware of the oversight of not amending the Cremation Regulations to allow NPs to complete cremation certificates and was “working as quickly as possible to remedy this”. She said the Ministry was currently in the process of informing stakeholders of its plan and timeline.
“In essence, not being able to do cremation certificates basically keeps in place the barrier to completing death certificates for over 80% of those I serve,” Michal Boyd said in a Facebook post to fellow Nurse Practitioners of New Zealand (NPNZ) members. “This development is so disappointing and frustrating. To feel that one of the last barriers to my practice in aged care was gone and to see it back again is very disheartening.”
She said apparently the cremation referee, who overseas cremation certificates, had let the Ministry of Health know of his concerns late last year about the regulations around cremation certificates being missed out.
NPNZ members shared Boyd’s frustration about the ongoing major barrier to NP practice, with one reporting that it cost her practice $90 every time it had to ask an outside GP to sign a death or cremation certificate for her patients. There was a call for action on the issue and concerns were expressed whether NPs would again to have wait years for this barrier to be removed.
Nursing Review sought comment on the NPs concerns from the Health Minister Dr David Clark and Ministry of Health. A spokesperson for the minister’s office said the Minister was aware of the issue and had asked the Ministry for a solution to the problem “which was inherited from the previous government”.
NB this article was updated on February 12 to include additional comment supplied in a revised response from the Ministry of Health and to clarify that it was the cremation regulations needed to be amended not the related legislation.
]]>