Following mediation in late January the New Zealand Nurses Organisation are waiting for the 20 DHBs to consider whether they can come back with a new offer by February 26.
The online petition was launched by NZNO in December after members voted to reject the DHBs’ initial multi-employer collective agreement (MECA).
NZNO Industrial Adviser Lesley Harry said nurses want to achieve pay rates and conditions that led to sustainable workforce and healthy workplaces.
She said any new offer needed to deliver improvements on the key issues – including a improved pay offer, safe staffing cand a firmer timeframe for pay equity – if it was to be accepted by members.
NZNO delegates Sarah Gilbertson and Karen Durham presented the petition to DHBs’ advocate Kevin McFadgen and said pay and conditions had to improve in order to sustain a quality health care service.
The pair said the issue was about recognising and rewarding a predominately female workforce. “The outcome of these negotiations is a reflection on our society and the value we place on health. Well supported health teams improve the health of all New Zealanders.”
NZNO has set up a series of MECA meetings between March 6-23 for its 27,000 registered nurse, enrolled nurse, midwife and health care assistant members covered by the NZNO/DHB MECA.
Prior to mediation the union indicated that it would not rule out using the March meetings to vote on industrial action, if a deal couldn’t be reached that it believed members would be ready to accept.
Late last month Health Minister David Clark told Nursing Review that he understood nurses’ and other health workers hopes for better salaries under the new Government but the was reality was that “not everyone’s expectations will be met”.
PETTION:
Dear District Health Board Chief Executives
‘Nurses, midwives and healthcare assistants are the heart of our public healthcare services. Their skills, hard work and compassion keep all New Zealanders happy, safe, and healthy. I support better pay and healthy workplaces in our public healthcare services for our precious nursing and midwifery teams. Please keep our local health services safe and sustainable by delivering our nurses a better deal.’
]]>
The United States’ CDC (Centers for Disease Control and Prevention) reported late last week (Feb 8) that levels of influenza-like-illness (ILI) had reached the peak of the 2009 H1N1 pandemic with unusually high numbers of hospitalisations in the 50-65 age group.
CDC reported that it didn’t believe the flu season had peaked in the US yet but the United Kingdom’s Public Health Service at the same time reported that flu numbers had stabilised and at this stage didn’t seem as severe as some other recent seasons. Both countries reported that the main flu strains circulating were flu A(H3N2) plus H1N1 strains and flu B strains.
Last year 66 per cent of district health board employees received the influenza vaccine – up on 61 per cent in 2014. Doctors remain the profession with the highest uptake of the flu vaccine with 72 per cent receiving the jab last year but nurses are now not far behind having increased their uptake from 59 per cent in 2014 to 68 per cent last year.
The DHB with the highest nurse vaccination rate remained Tairawhiti at 84 per cent followed by Auckland, Northland and Waikato all at 81 per cent. The DHBs with the lowest nurse vaccination rates were Wairarapa (47%), Lakes (49%) and MidCentral (55%).
Midwives remain the profession with the lowest uptake which fell from a high of 59 per cent in 2015 to 54 per cent last flu season.
The Immunisation Advisory Committee (IMAC) and Ministry of Health are again pointing out that healthcare workers can transmit influenza without knowing they are infected as the flu doesn’t always cause symptoms or make people unwell.
Data from the Southern Hemisphere Influenza and Vaccine Effectiveness Research and Surveillance (SHIVERS) study, based in Auckland, suggest that four out of five children and adults (80%) with flu were asymptomatic. And an earlier study – following the 2009 ‘swine flu’ pandemic in New Zealand – found almost one quarter of the adults who reported that they had not had influenza in 2009 were tested and found to have been infected by the H1N1 virus that caused the pandemic.
The New Zealand-based Southern Hemisphere Influenza and Vaccine Effectiveness, Research and Surveillance (SHIVERS) study has indicated that flu vaccine effectiveness in New Zealand is around 50 per cent or more.
Four strain vaccine available this year
Pharmac has confirmed that this year it will be funding for the first time a flu vaccine targeted at four strains of the flu virus rather than the usual three strains.
Two forms of quadrivalent vaccine will be funded from March 1 with Influvac Tetra funded for eligible people aged three years and over and another vaccine, Fluarix Tetra, funded for eligible children aged 6 to 35 months.
Pharmac deputy medical director Dr Bryan Betty says the four-strain vaccine will offer additional protection against influenza in 2018, and into the future.
Pharmac negotiated long-term supply with Mylan in 2016, including provision for a four-strain vaccine once it was approved for use by Medsafe. This has now occurred.
The funded vaccines will both contain the strains of influenza virus specified by the World Health Organisation for the 2018 Southern Hemisphere influenza season which are:
- an A/Michigan/45/2015 (H1N1)pdm09-like virus;
- an A/Singapore/INFIMH-16-0019/2016 (H3N2)-like virus; and
- a B/Phuket/3073/2013-like virus
- a B/Brisbane/60/2008-like virus
CDC Acting Director Dr. Anne Schuchat said last week that it was known that flu vaccines can often have lower effectiveness against H3N2 viruses but added that “however some protection is better than none” against the virus strains which were often linked to more severe illness – especially among children and people aged 65 and older.
Stock of the New Zealand seasonal influenza vaccine is typically available from early March until 31 December each year.
The exact start date for the 2018 seasonal influenza vaccination programme will be notified by the Ministry of Health in due course. The Fluarix Tetra vaccine for children under 3 years is likely to be available from mid-April 2018.
7876IMAC 2017 FLU_infographic_audio from Theo Brandt on Vimeo.
]]>Waikato DHB’s acting chief executive Derek Wright has asked for a review of the previous CEO Nigel Murray’s policy of requiring non-vaccinated health workers to wear masks while delivering patient care.
Murray brought the unpopular VOM (vaccinate or mask) policy with him from his old employer, British Columbia’s Fraser Health Authority where the policy had successfully withstood a union legal challenge.
Waikato introduced the hardline policy in 2015 – including suspending two unvaccinated nurses – and saw its nurse vaccination rate jump from 52% in 2014 to 81% in 2015, 80 per cent in 2016 and 81 per cent again last year.
The New Zealand Nurses Organisation has been on the record that while the organisation was quite clear it encouraged nurses and other members to get the seasonal flu vaccine, it also had “significant concerns” about the co-ercive nature of a VOM policy.
Waikato’s staff immunisation rate has never surpassed Tairawhiti DHB whose positive campaign – centred around a focused week-long campaign into every DHB department followed by catch-up clinics near the staff cafeteria – has kept the DHB at the top of the vaccination tables for four years with 84 per cent of both nurses and overall staff getting the flu jab last season. Tairawhiti also had the highest percent of ‘other’ DHB staff getting immunised at 90 per cent and the highest percentage of midwives with 88 per cent.
A Waikato spokesperson said the DHB had decided it was timely to revisit the VOM policy to see whether it was working. “Our Infection Control Committee will be looking at the evidence and research around masking and make a recommendation to the Executive. It could mean the policy is amended, or it could remain,” said the spokesperson. She said Wright was keen to work with staff and find the best solution for the DHB’s staff which also kept patients safe. “Obviously getting immunised and staying home if you are sick is the best protection for everyone.”
The DHB’s acting chief executive initially trained as a general nurse and then mental health nurse in the United Kingdom and worked in a variety of mental health management positions in the UK, New Zealand and Australia before joining Waikato in early 2016 as the DHB’s mental health director.
]]>The NZNO and negotiating team for the 20 District Health Boards entered mediation on January 31 after NZNO’s DHB nurses, midwives and health care assistants voted to reject the initial pay offer made in November.
The NZNO negotiating team said in an update that it presented the findings of its online member survey to last week’s mediation, including that members wanted an increased pay offer, safe staffing, a shorter term for the agreement (the original offer was for a 33 month term), and a firmer timeframe for pay equity.
“We were clear that any revised offer will require additional funding as trading off improvements from the previous offer would not be acceptable,” said the update to the about 27,000 members that will be covered by the new DHB/NZNO MECA (multi-employer collective agreement).
The original pay offer – a two per cent increase, backdated to November 6, for the majority of nurses and midwives covered by the MECA and further two per cent pay rise in August 2018 and August 2019 – was widely viewed by nurses as too little too late. Members were also divided on how quickly the initial offer’s agreement to start negotiating a pay equity settlement would deliver results for nurses.
The NZNO negotiators said the DHBs were now “going to look at their ability to reconstruct an offer that addresses NZNO concerns”. The DHBs were due to report back to NZNO by February 26 and members were to be updated on the outcome prior to a series of member meetings running from March 6 to March 23.
“Should DHBs agree to an improved offer the update will include the detail the offer for members to vote on at the meetings,” said the update.
Prior to mediation the union indicated that it would not rule out using the March meetings to vote on industrial action, if a deal couldn’t be reached that it believed members would be ready to accept.
Late last month Health Minister David Clark told Nursing Review that he understood nurses’ and other health workers hopes for better salaries under the new Government but the was reality was that “not everyone’s expectations will be met”.
]]>Survey respondents were also found to be divided over what gains the the proposed pay equity process –due to start after the new contract is settled – would deliver and how quickly.
The online survey followed the New Zealand Nurses Organisation’s District Health Board members voting to reject the 20 DHB’s MECA (multi-employer collective agreement) offer with strong social media feedback that many felt the offer fell short of reflecting the skills and increasing workloads of nurses.
The union and employer negotiating teams were starting mediation today with the union not ruling out a vote on industrial action if a deal can’t be reached that members are ready to accept.
In a survey summary to members the NZNO negotiating team said safe staffing was also reiterated as a key issue by members concerned about continuing to work “under-staffed and under pressure”.
Other issues highlighted was that members felt back pay or a lump sum was important (the current agreement expired on July 31 last year), and most members favoured a two year term (the original offer was for a 33 month term).
The initial pay offer included an agreement to start negotiating a pay equity settlement and the survey found that 80 per cent of respondents backed a strategy to have pay parity with medical radiation technologists (MRTs) and allied health professionals. The survey showed members were divided on whether the pay equity could deliver but survey respondents had indicated that a better base scale pay offer could increase their support of the proposed pay equity process.
A petition seeking public support for a better pay offer for district health board nurses had also reached nearly 13,800 signatures as mediation got underway today.
]]>
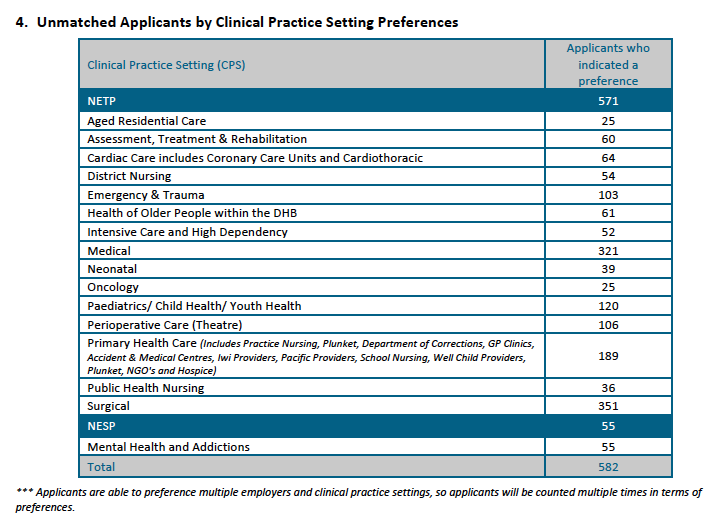
Overall 582 (43 per cent) of the 1389 applicants found out on November 22 last year that they were unsuccessful in the first job match. While most of the unsuccessful applicants were seeking surgical or medical nursing positions, the latest ACE report shows a high proportion of graduates seeking mental health and addictions, aged residential care and primary health care roles were also unsuccessful.
Hilary Graham-Smith, professional services associate manager for the New Zealand Nurses Organisation, said yesterday that hundreds of graduates missing out on jobs was unacceptable considering the national nursing workforce goal was 100 per cent placement by 2018.
The ACE Nursing Algorithmic Match Report provides a breakdown of the 913 jobs on offer and the 775 new graduates matched with jobs on November 10 in the end-of-year round of the ACE new graduate nurse job-matching process. In all, 57 per cent of the 1389 applicants found out on November 22 that they had been offered positions on Nurse Entry to Practice (NETP) and Nurse Entry to Specialist Practice (NESP) programmes. At least 138 positions were still to be filled as at November 10 and historically more graduates are also offered jobs over the summer break as vacancies arise leading up to NETP and NESP programmes getting underway in late January/early February this year.
Graham-Smith said the overall trend in new graduate jobs for nurses showed no significant increase. “This is not the case in medicine: every new graduate doctor has a place on an entry programme. This speaks to the chronic under-investment in nursing and a complete lack of progress on guaranteeing all new graduates of a place on a programme by 2018,” she said.
She said Health Workforce New Zealand head Des Gorman has called it a “perfect storm” as nursing has gone through a long period of under recruitment and training. “This matches our research on nursing employment. We have an aging workforce and over-50s leaving. We are simply not attracting, training or retaining enough nurses to future-proof our healthcare services,” she said.
Concern was expressed last year about shortages and high vacancies for acute mental health nursing positions. The ACE match report shows that 55 of the 210 applicants who expressed interest in the NESP programmes for mental health and addiction nurses were unsuccessful.
In addition, 25 of the 39 nurses who indicated a preference for aged residential care and 189 of the 359 who were keen on primary healthcare positions (which include practice nursing, prison nursing, Plunket and hospice positions) were unsuccessful in the first job round.
The DHBs in which it was hardest to get jobs (i.e. which turned away the highest proportion of applicants who had put that DHB down as their first preference) included Hutt Valley, Mid-Central, Capital & Coast, Waikato, and Auckland, which accepted between 28 to 42 per cent per cent of the first-preference applicants (see table at bottom of article for the number of jobs on offer).
Ethnicity and second-time-around job rates
The percentage of Māori and Pacific nurse graduates offered jobs on November 10 was again slightly higher than the average job success rate at 70 per cent (145 of 206 applicants) and 63 per cent (54 of 85 applicants) respectively, compared with 57 per cent for all applicants.
Asian applicants were once again the least successful in obtaining job offers, with just 39 per cent (86) of the 220 applicants being offered a job in the first round. The job rate for the ‘other’ ethnicity category (largely Pākehā/European) was the same as for all applicants – 57 per cent – with 490 of the 846 applicants being successful.
The vast majority of the November applicants were first-time-round applicants and 60.5 per cent of those applicants were successful. Just over 35 per cent of the 115 second-time-round applicants were successful and 26 per cent of the 49 applicants applying for a third time or more.
The ACE Nursing Intake Summary Report was prepared by the agency TAS (formerly known as DHB Shared Services), which owns ACE Nursing on behalf of the 20 DHBs.
The next ACE report is not due until after the National Talent Pool, from which DHBs can employ unmatched new graduate applicants, closes in late June.
Report author Kamini Pather said there was a lot of dynamic change to ACE daily statistics as applicants get offered jobs, withdraw from the talent pool for other reasons or change their preferences. This meant there were only two points in the recruitment cycle where stable and reliable data could be extracted. Those were at the time of the electronic match (November 10) and once the National Talent Pool and end-of-year intake closes, which is about seven months later in late June.
| Employer | Positions submitted to ACE Nursing for End of Year Match | Total Applicants Matched to Employer (as at Nov 10 2017)
|
| Auckland DHB | 107 | 79 |
| Bay of Plenty DHB | 49 | 49 |
| Canterbury DHB | 112 | 100 |
| Capital & Coast DHB | 65 | 56 |
| Counties Manukau DHB | 97 | 80 |
| Hawke’s Bay DHB | 32 | 29 |
| Hutt Valley DHB | 14 | 14 |
| Lakes DHB | 17 | 17 |
| MidCentral DHB | 19 | 14 |
| Nelson Marlborough DHB | 37 | 37 |
| Northland DHB | 24 | 22 |
| South Canterbury DHB | 15 | 13 |
| Southern DHB | 58 | 53 |
| Tairawhiti DHB | 10 | 10 |
| Taranaki DHB | 23 | 21 |
| Waikato DHB | 94 | 66 |
| Wairarapa DHB | 4 | 4 |
| Waitemata DHB | 97 | 78 |
| West Coast DHB | 5 | 4 |
| Whanganui DHB | 18 | 18 |
| Southern Cross Hospitals – Auckland | 7 | 3 |
| Southern Cross Hospitals – Midland (Waikato & BoP) | 3 | 3 |
| Southern Cross Hospitals – Southern (Christchurch) | 6 | 5 |
| Total | 913 | 775 |
]]>
Health Minister David Clark says he understands nurses’ and other health workers’ hopes for better salaries under the new Government, but the reality is that “not everyone’s expectations will be met”.
He was responding to questions from Nursing Review and online health hub Health Central about New Zealand Nurses Organisation members rejecting the 20 district health boards’ pay offer of roughly two per cent a year, amidst expectations that the incoming Government may be more open to funding a more “respectful” offer.
Minister for Women Julie Anne Genter, who is also Associate Minister of Health (but in that capacity has no responsibility for wage settlements), says she is aware that nurses’ expectations are high and meeting everybody’s expectations poses “fiscal challenges” as there is a lot of investment that the new Government needs to catch up on.
Clark said he would not comment on the negotiations, which are due to go to mediation at the end of the month – with NZNO not ruling out industrial action if a better offer was not reached – or pre-empt the mediation outcomes.
“But I can understand firstly why those nurses might have hopes of better things. This is a government that wants to see a more sustainable health sector. We don’t intend to run it down like our predecessors did. We want to ensure there are healthy workplaces and safe staffing and more sustainable funding over time.”
He said he needed to better understand why the NZNO negotiating team thought the initial pay offer would be accepted by members and why it was rejected.
“But the public also has an expectation based on the priorities outlined and the promises made that there will be more services delivered.”
“So the money that we pledged to put into healthcare won’t all go into salary raises,” said Clark. “Not everyone’s expectations will be met. I think that is the reality and I think we need to be upfront about that. But a Labour Government recognises the need to have a sustainably funded workforce and the need to make sure we have safe staffing and healthy workplaces.”
Nurses and midwives underpaid
Genter said as Minister for Women her number one priority was new pay equity legislation and working to close the gender pay gap in the public service.
“Female-dominated professions like midwives and nurses have structurally lower pay,” said Genter. “Those professions have been underpaid and undervalued because they are female-dominated.”
She said where there were MECAs (multi-employer collective agreements) for specialists or doctors the gender pay gap had disappeared, because so many more women were pursuing medicine and becoming specialists.
“But across the health workforce it is not necessarily the case and there is still more work to be done to rectify the pay gap.” She is aware of the NZNO’s pay equity claim for its DHB nurses, midwives and health care assistants. She said such pay equity claims are not her responsibility alone, but as Minister for Women she is working with other ministers on pay equity legislation to progress such claims (see below).
“Obviously this government is very supportive of closing the gender pay gap and lifting pay for the lowest paid workers, and valuing all of the professions that add so much to life in Aotearoa – we can’t do without them.”
Genter, in her role as Associate Minister of Health, spoke to Health Central about her two new delegations for health – population health (built environment) and climate change – along with women’s health, sexual health and disability services.
Next step to new pay equity legislation
This week Genter, in her role as Minister for Women, and Iain Lees-Galloway, the Minister for Workplace Relations and Safety, announced the reconvening of the Joint Working Group on Pay Equity Principles as the first step to new pay equity legislation.
The original group was set up in 2015 to develop principles to guide pay equity implementation, but Galloway said these principles had been ‘undermined’ by the pay equity bill introduced in July last year by the former government, which would have made pay equity claims tougher for women. The bill was scrapped by the incoming government in November.
The new working group has been charged with considering the issues around how to determine the merit of a pay equity claim and how to select appropriate male comparative professions/trades to compare the pay rates of women workers who lodge pay equity claims.
The group, facilitated by Traci Houpapa, meets today, January 24, and is due to make its recommendations to Ministers by the end of February. “Once we receive the recommendations, we will work to develop pay equity legislation which we expect to introduce mid-2018,” said Genter.
The tripartite partners include government representatives, unions (led by the New Zealand Council of Trade Unions) and employers (led by BusinessNZ and the Employers and Manufacturers Association).
]]>In mid-December the New Zealand Nurses Organisation (NZNO) announced that its nurse, midwife and healthcare assistant DHB members had voted to reject the proposed new DHB MECA (multi-employer collective agreement) during 400 meetings held across the country.
The pay offer – a two per cent increase, backdated to November 6, for the majority of nurses and midwives covered by the MECA, and further two per cent pay rise in August 2018 and August 2019 had been widely criticised in social media by some of the 27,000 NZNO members covered by the proposed deal as being too low and not adequately reflecting the pressure and stress they had worked under in recent years (see details of the rejected offer here).
In its update to members on December 13, the NZNO negotiating team said the rejection of the proposed MECA showed that DHB members believed a “better offer was worth the very serious consideration of possible industrial action”.
It said the team would “take every opportunity in front of us” to achieve a better offer through mediation (due to begin January 31) without resorting to industrial action. But it had scheduled a series of meetings starting in late February to update DHB members on the negotiation’s progress and those meetings could be used to hold a ballot on industrial action.
“Should industrial action occur, we will work with DHBs to provide essential services for people who need them,” said the MECA update. “We are aware of your professional commitment to your patients and although it hasn’t happened for a long time, we have experience of industrial action and balancing the two.”
A spokesperson for the DHBs’ negotiating team has yet to respond to Nursing Review’s request for comment.
NZNO industrial advisor Chris Wilson said participation is going well in its online survey of DHB members. The survey is being used to get formal confirmation from DHB members of the anecdotal feedback negotiators had received on what were the major issues that members wanted addressed when the negotiations go to mediation on January 31. The survey went online just before Christmas and is due to close at 4pm on Thursday, January 18.
Wilson said the survey did not include a question on whether to pursue industrial action if mediation failed to meet a resolution, and instead focused on getting formal feedback on what was needed to reach a MECA deal that members would accept.
She said the NZNO negotiators at this point were very much committed to the mediation process. “Obviously we will see what occurs on Jan 31.” A reserve day for mediation has also been set for early February.
“Industrial action does remain a possibility if we’re not able to secure an outcome through mediation that members are comfortable with,” said Wilson. But she said it was hopeful that once employers saw the issues highlighted by members in its online survey the negotiations “might make some grounds”.
The December 13 MECA update to NZNO DHB members said that it understood that the members key reasons for rejection were as follows:
- The two per cent pay increase was not enough to recognise the hours of unpaid overtime, missed breaks, stress and burnout that members had experienced as a result of the persistent health funding shortages over the last nine years.
- There wasn’t enough clarity about the amount and timing of any pay increases due to the planned pay equity process.
- Members were concerned that the nearly three-year MECA term meant that they would get left behind relative to other groups. Especially if the pay equity process didn’t deliver a quick result.
- The apparent lack of a guarantee of funding or staffing available to respond to the demand created by the implementation of the safe staffing process.
]]>
The DHBs’ offer – that had been endorsed by the New Zealand Nurses Organisation (NZNO) negotiating team – had been widely criticised in social media by some of the 27,000 nurses, midwives and health care assistant members of NZNO covered by the proposed deal.
The pay offer – a two per cent increase, backdated to November 6, for the majority of nurses and midwives covered by the MECA and further two per cent pay rise in August 2018 and August 2019 –appeared to be seen as too little too late. The offer also included a small lump sum of $350 and an agreement in principle by the 20 DHBs to progressing a pay equity claim with negotiations to begin in the year. (See details of the rejected offer here)
Harry acknowledged that the members rejection reflected their views that the offer “failed to respect nurses, midwives and health car assistants and the huge effort and value they bring to patients and our communities”. She said the next formal step was likely to be mediation between NZNO and the DHBs. Nursing Review has sought comment from the DHBs’ negotiating team spokesperson but they had not responded at this point.
Nurses on social media had expressed disappointment and frustration that the DHBs’ offer was about or below inflation, it didn’t reflect growing pressures and responsibilities placed on nurses in the workplace and it wouldn’t reinstate the pay relativity lost by this year’s $2 billion pay equity settlement to care and support workers in the aged care and disability sector.
Harry also acknowledged that it appeared members did not have confidence that the agreement in principle by DHBs to start pay equity negotiations would see extra money in their pockets soon.
“I think members lost a lot of trust and confidence over the years of austerity,” said Harry. She said the negotiating team had supported the DHBs pay offer on the basis of the DHBs seeing merit in the pay equity claim and the new government’s support of pay equity.
“The negotiating team were certainly more optimistic (about the likelihood of getting a pay equity settlement) than the feedback we’ve got from members,” said Harry. “And we will take the opportunity between now and we get to meet with our members next to fully inform them of what the pay equity process is.”
Harry would not disclose whether voters resoundingly or narrowly rejected the offer. But she did say it was pleased with the turnout at the 400 meetings held across DHBs in the past few weeks which was probably the highest turnout in more than a decade.
Posters on social media in the past few weeks – both for and against the offer – had called on nurses to turn up to meetings to be briefed on the details and make their voice count.
Harry said anecdotally it had a sense of what offer might be acceptable for members but it was first going to canvas members, via an electronic survey, so the negotiating team could be “absolutely confident” on what members would be prepared to ratify. The aim was to post the survey before Christmas.
She said the timing of the mediation was not known yet but NZNO was setting up a series of member meetings in late February that would either be follow-up meetings to discuss next steps or “all going well” might have a ratifiable offer to put to members by then.
“Of course nurses and DHB employers will be doing their best to reach an employment agreement acceptable to both parties,” said Harry.
“Consideration of industrial action will only occur if NZNO and DHBs cannot achieve a resolution of the issues members have raised,” Harry confirmed.
]]>
Victoria University researcher Dr Helen Rook’s recently completed PhD research found Kiwi nurses felt conflicted and anxious at being unable to deliver care true to their nursing values because of pressures on the ward to discharge patients quickly, keep-up the paper work and keep costs down.
She said the nurses’ response– sometimes conscious and sometimes not – was to focus on essential duties like documentation and nursing tasks as a coping strategy. Sometimes this also lead to nurses cutting short patient conversations, ignoring call bells and in other ways withdrawing from their patients to protect themselves emotionally.
Rook’s PhD research – prompted in the wake of the inquiry into patient neglect in Mid-Staffordshire – involved spending 300 hours observing nurses on medical wards in three district health boards, multiple interviews, checking nurse sensitive indicator statistics (like falls and pressure injuries), and measuring burnout levels. She concluded that the conflict that the nurses felt – between their personal and professional values and how they actually were able to practice nursing because of the constraints of modern healthcare – caused anxiety, exhaustion, cynicism and burnout.
Building and supporting nursing leadership at the ward level upwards was one recommendation by Rook to help nurses speak up and act on their concerns. Another was for district health board and other healthcare providers to put in place strategies to help mitigate the organisational dysfunction and financial constraints that lead to nurses feeling unable to consistently deliver compassionate, clinically competent care.
Withdrawing from patients a coping strategy for conflicted nurses
“In all of the wards the nurses said they were practising team nursing and yet there was very little evidence of that,” said Rook. Instead they were observed to be mostly focussed on tasks and “getting things done”. “They are very skilful at that,’ said Rook. “In order to protect themselves they use defensive strategies to protect themselves from anxiety.”
She said the conflicted nurses also used the coping strategy of withdrawing a little bit from the patients they were caring for. So they tried not get caught in conversations with patients by using strategies like giving a quick smile. “Or say ‘I’ll be with you in a minute’ and then pull themselves away as they know they have all this other stuff they need to get done.”
Rook said she also observed more overt withdrawal by busy nurses. “I watched nurses walking past patients who were calling out for help, and call bells that were unanswered, not because nurses were uncaring but because they had so many other things to do, to comply with.”
When she spoke to nurses about the organisational values at their DHBs – and the DHB’s strategies for improving patients care – she said a number expressed cynicism that while DHBs talked about focusing on partnership and respect most improvement projects were actually about discharging patients quicker, balancing the budget and ensuring the required documentation was done. She said there was also a sense that the DHB’s emphasis on economics and managerialism was becoming more prevalent not less.
But she added that for her Phd she drew on the iconic nursing research carried out in a London hospital in the late 1950s by Isabel Menzies, who wrote about how nurses de-personalised patients to protect themselves from the anxiety of their work.
“That’s a long time ago – we’re 2017 now – but a lot of things that she found in that research I also found in my research. Not a lot has changed in healthcare in the intervening years really…”
Be consciously present not emotionally numb
“Nurses go into the profession with an assumption that they will be caring for people who are sick, taking a moment to talk with them and build caring relationships,” said Rook.
But said the current culture didn’t allow for that and DHB’s managerial imperatives to get patients out of hospital quickly, combined with financial constraints, meant that it just wasn’t possible. So nurses often responded by focussing on doing the essential nursing tasks.
“I think there is a bit of guilt in that we focus on tasks,” said Rook. “I don’t think it’s such a bad thing if we do. Because that is what the public expect – they expect us to be able to do things for them.”
Rook said if the reality was that nurses’ coping strategy for pressured workloads was to focus on tasks, then nurses should take ownership of this new reality. They needed to be vocal about the type of nursing care they were able to deliver, and why, and then deliver the task excellently.
“We need to be very clear that ‘okay we are going to focus on a task but we are going to be excellent in that task and in our interactions with people….even if is only a minute or two.”
She said nurses need to aim to be fully present with their patient even if “just doing a task” as that would be much more beneficial therapeutically.
“We need to be consciously present rather than emotionally numb in our patient interactions.”
But in the long-term she said it was imperative that nurses on the frontline were supported to build leadership skills and find their voice so the culture was changed and they could provide the nursing care that matched their personal and professional values. Also organisations had to introduce strategies that removed the constraints currently preventing nurses from delivering that care.
Rook, who is currently the Programme Director at the Graduate School of Nursing, Midwifery and Health at Victoria University of Wellington, graduates next week with her PhD in nursing.
She has a background in critical care nursing in the United Kingdom, Ireland and New Zealand, and has worked as a nursing academic in New Zealand and Ireland delivering undergraduate and post-graduate education.
]]>