A Plunket spokeswoman Jen Riches last week confirmed that Plunket was proposing disestablishing 53 positions in the Central region’s – which covers the North Island south of Auckland – and replacing them with 34 positions. The positions relate to administrative, leadership, and community services roles with Plunket’s government-funded Well Child nursing services not included in the Central region restructuring proposal but the New Zealand Nurses Organisation (NZNO) says Plunket does propose moving from four clinical services manager (i.e nurse leader) positions to two.
This month Plunket chair Christine Lake has also sent out a public appeal seeking “urgent support to raise $150,000 by 5th March 2018 so Plunket can keep life-changing community programmes running”. She said childcare and parenting groups were not easily accessible in high need communities and Plunket trained and supported volunteers with the skills needed to develop playgroup and manage other programmes that led to “more supportive, connected communities”.
The Central region proposal follows Plunket consolidating its regional societies into a single entity last year. Riches said Plunket was focused on providing a “consistent range of community services” to families across the country including how to “best support consistent and equitable service delivery” in the central region where Plunket would be serving around 19,00 new babies and their families in the coming year.
The proposal is for 53 staff to have their roles disestablished and to be replaced with 34 roles – 18 of these to be re-confirmed roles, 15 contestable roles and one newly created role. Riches said the proposal was “by no means a decision” and there was still some way to go before decisions were made.
Chris Wilson, NZNO’s industrial advisor for the primary health care sector said it was currently in a “robust consultation” with its affected members before making a submission to Plunket. She said a number of the job changes were due to the Central Region proposing reducing the number of operating areas to two. She said this included reducing the number of clinical services managers (nurse leadership positions) from four to two while having the same number of clinical leaders and nurses to manage. The proposal also included reducing the number of administration team leaders from 6 to two and a reduction in administrator roles.
Wilson said it appeared the changes would lead to less people managing more staff in a centralised structure.
“Our initial concerns would therefore be sustainable workload management for the staff affected and equitable access for rural and smaller communities to appropriate Plunket services.”
In late 2016 Plunket voted at its national annual general meeting to consolidate its 14 area societies into a single national charitable trust by the end of 2017 to enable Plunket “to deliver more equitable outcomes for its community services” and manage its property more efficiently. Lake said at the time that while Plunket delivered Well Child services in most part of the country. through its Ministry of Health contracts, its other services – such as parenting education programmes and play groups – were “not being universally provided because of a lack of local volunteers and fundraising”. She said as a charity Plunket relied on the effort and generosity of supporters to keep delivering its services that weren’t funded through government contracts.
NB article updated at 3pm January 29 to include NZNO comment
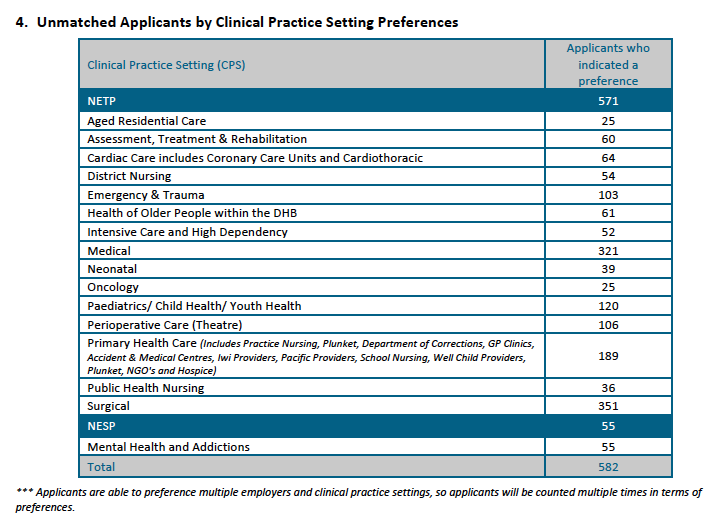
]]>Overall 582 (43 per cent) of the 1389 applicants found out on November 22 last year that they were unsuccessful in the first job match. While most of the unsuccessful applicants were seeking surgical or medical nursing positions, the latest ACE report shows a high proportion of graduates seeking mental health and addictions, aged residential care and primary health care roles were also unsuccessful.
Hilary Graham-Smith, professional services associate manager for the New Zealand Nurses Organisation, said yesterday that hundreds of graduates missing out on jobs was unacceptable considering the national nursing workforce goal was 100 per cent placement by 2018.
The ACE Nursing Algorithmic Match Report provides a breakdown of the 913 jobs on offer and the 775 new graduates matched with jobs on November 10 in the end-of-year round of the ACE new graduate nurse job-matching process. In all, 57 per cent of the 1389 applicants found out on November 22 that they had been offered positions on Nurse Entry to Practice (NETP) and Nurse Entry to Specialist Practice (NESP) programmes. At least 138 positions were still to be filled as at November 10 and historically more graduates are also offered jobs over the summer break as vacancies arise leading up to NETP and NESP programmes getting underway in late January/early February this year.
Graham-Smith said the overall trend in new graduate jobs for nurses showed no significant increase. “This is not the case in medicine: every new graduate doctor has a place on an entry programme. This speaks to the chronic under-investment in nursing and a complete lack of progress on guaranteeing all new graduates of a place on a programme by 2018,” she said.
She said Health Workforce New Zealand head Des Gorman has called it a “perfect storm” as nursing has gone through a long period of under recruitment and training. “This matches our research on nursing employment. We have an aging workforce and over-50s leaving. We are simply not attracting, training or retaining enough nurses to future-proof our healthcare services,” she said.
Concern was expressed last year about shortages and high vacancies for acute mental health nursing positions. The ACE match report shows that 55 of the 210 applicants who expressed interest in the NESP programmes for mental health and addiction nurses were unsuccessful.
In addition, 25 of the 39 nurses who indicated a preference for aged residential care and 189 of the 359 who were keen on primary healthcare positions (which include practice nursing, prison nursing, Plunket and hospice positions) were unsuccessful in the first job round.
The DHBs in which it was hardest to get jobs (i.e. which turned away the highest proportion of applicants who had put that DHB down as their first preference) included Hutt Valley, Mid-Central, Capital & Coast, Waikato, and Auckland, which accepted between 28 to 42 per cent per cent of the first-preference applicants (see table at bottom of article for the number of jobs on offer).
Ethnicity and second-time-around job rates
The percentage of Māori and Pacific nurse graduates offered jobs on November 10 was again slightly higher than the average job success rate at 70 per cent (145 of 206 applicants) and 63 per cent (54 of 85 applicants) respectively, compared with 57 per cent for all applicants.
Asian applicants were once again the least successful in obtaining job offers, with just 39 per cent (86) of the 220 applicants being offered a job in the first round. The job rate for the ‘other’ ethnicity category (largely Pākehā/European) was the same as for all applicants – 57 per cent – with 490 of the 846 applicants being successful.
The vast majority of the November applicants were first-time-round applicants and 60.5 per cent of those applicants were successful. Just over 35 per cent of the 115 second-time-round applicants were successful and 26 per cent of the 49 applicants applying for a third time or more.
The ACE Nursing Intake Summary Report was prepared by the agency TAS (formerly known as DHB Shared Services), which owns ACE Nursing on behalf of the 20 DHBs.
The next ACE report is not due until after the National Talent Pool, from which DHBs can employ unmatched new graduate applicants, closes in late June.
Report author Kamini Pather said there was a lot of dynamic change to ACE daily statistics as applicants get offered jobs, withdraw from the talent pool for other reasons or change their preferences. This meant there were only two points in the recruitment cycle where stable and reliable data could be extracted. Those were at the time of the electronic match (November 10) and once the National Talent Pool and end-of-year intake closes, which is about seven months later in late June.
| Employer | Positions submitted to ACE Nursing for End of Year Match | Total Applicants Matched to Employer (as at Nov 10 2017)
|
| Auckland DHB | 107 | 79 |
| Bay of Plenty DHB | 49 | 49 |
| Canterbury DHB | 112 | 100 |
| Capital & Coast DHB | 65 | 56 |
| Counties Manukau DHB | 97 | 80 |
| Hawke’s Bay DHB | 32 | 29 |
| Hutt Valley DHB | 14 | 14 |
| Lakes DHB | 17 | 17 |
| MidCentral DHB | 19 | 14 |
| Nelson Marlborough DHB | 37 | 37 |
| Northland DHB | 24 | 22 |
| South Canterbury DHB | 15 | 13 |
| Southern DHB | 58 | 53 |
| Tairawhiti DHB | 10 | 10 |
| Taranaki DHB | 23 | 21 |
| Waikato DHB | 94 | 66 |
| Wairarapa DHB | 4 | 4 |
| Waitemata DHB | 97 | 78 |
| West Coast DHB | 5 | 4 |
| Whanganui DHB | 18 | 18 |
| Southern Cross Hospitals – Auckland | 7 | 3 |
| Southern Cross Hospitals – Midland (Waikato & BoP) | 3 | 3 |
| Southern Cross Hospitals – Southern (Christchurch) | 6 | 5 |
| Total | 913 | 775 |
]]>
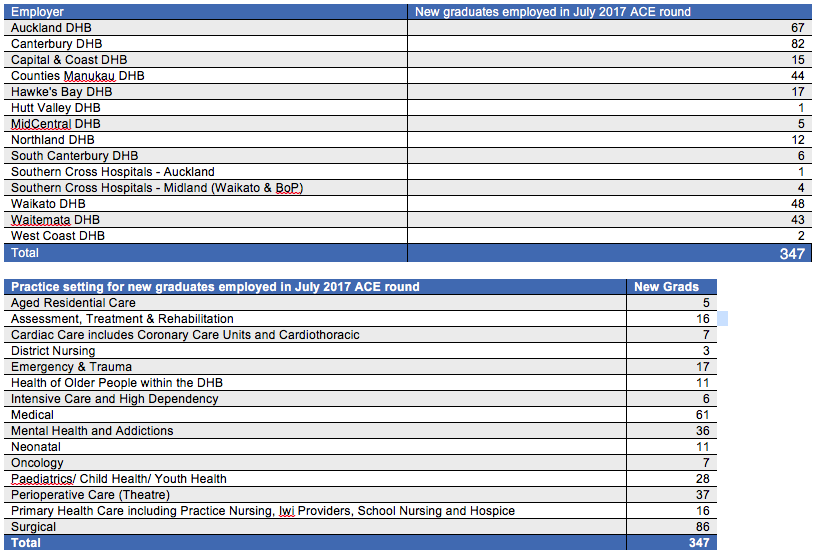
Statistics released by the Ministry of Health showed that 347 of the initial 701* new graduate applicants were matched with jobs in the July round of ACE nurse graduate job clearinghouse. This is equivalent to 49.5 per cent – slightly down on the 53 per cent success rate last year when 332 of 648 applicants were successful.
Nearly 390 positions had been available in the mid-year job round across 12 of the 20 district health boards (see table below) and six positions in two Southern Cross Hospitals – which was up on the 350 jobs on offer at the same time last year.
In the latest round, jobs were initially offered to 354 candidates but seven candidates declined positions or advised ACE that they had failed state finals. But by the end of August a further 48 candidates from the remaining talent pool had been matched with jobs, bringing the number of successful mid-year candidates up to 395 (56.3%) and leaving about 262 applicants still in the job-hunting pool.
Chief Nursing Officer Jane O’Malley said about 600 of the approximately 1800 New Zealand-trained nurses registered each year graduated in July and the goal was for all graduates to be employed. Data gathered since the ACE process began in 2012 found that 40-60 per cent are offered jobs before they have their state final exam results, 60-70 per cent are employed within five months and almost all are employed with 12 months.
O’Malley said in the latest round 251 (60 per cent) of the 421 applicants who had just sat their state finals were offered jobs in the initial round. A further 27 were employed from the talent pool, making a total of 278 (66 per cent) being employed within two months.
The majority of the latest ACE job offers were from across the three DHBs in the Auckland region (154), followed by 82 jobs offered by Canterbury DHB and 48 by Waikato DHB. Surgical (86) and medical (61) were the most common positions filled, followed by perioperative (37) and mental health and addictions (36). (See more details in tables below.)
In total, 466 of 701 initial applicants were applying to ACE for the first time (the 421 July graduates plus 45 graduates from earlier cohorts) and of these 276 (60 per cent) were successful in the first round. This is slightly down on the 62 per cent success rate in the initial round for first time applicants at the same time last year.
Seventy (33 per cent) of the 211 applicants who were applying for jobs through ACE for the second, third or more times were successful in their latest attempts. The ACE data also indicates that 20 (4 per cent) of the graduates from July last year are still seeking new graduate positions through ACE.
*N.B. Forty-four applications were withdrawn prior to the job-matching process, either because they had gained employment or failed to complete their degrees, bringing the total number of applicants taking part in the round down to 657. The same time last year 27 applicants withdrew before the match, bringing application numbers for the match down from 648 to 621.
]]>
The recruitment consultant for ACE Nursing knows this is easier said than done.
“The application timeframe is very tight as it’s leading up to exams and often during your final clinical placement,” says Campbell. But time spent on applying for your first nursing position is time well invested.
Since 2012 all students seeking Nurse Entry to Practice (NETP) or New Entry to Specialist Practice (NESP) graduate training programme places go through the centralised, online ACE Nursing recruitment process.
Each year the ACE (Advanced Choice of Employment) team visits nursing schools around the country to talk third-year students through the application process and point them towards further information and advice available on the ACE Nursing website (see links below). “We try and take as much stress out of it (the application process) as possible,” says Campbell
He says if there is one area where first time applicants do make mistakes it is not allocating enough preparation time to complete the documentation required
Though registering too early on the ACE website – that is before ACE applications formally open – is not recommended either. It just heightens the risk you will forget your password. “Students are quite notorious for doing that,” laughs Quentin
So he encourages you to wait until the opening date, which for the end-of-year applications will be Wednesday 16 August, before creating a login on the ACE site.
Cover letters need time
What you should not be leave to the last minute is preparing the documents required for your application – particularly your resume (CV) and covering letters.
Campbell says if you have all the documents and information required on the checklist it takes about half an hour to lodge an ACE application.
What takes longer than many students realise is finishing your resume (CV) and writing up to three covering letters. “I think a lot of people take that for granted. What I advise students is that resumes will take a little bit of time and you need to choose your own way to present that document to your employers.”
“But it really is the cover letters that are taking the most amount of time for the students.” Cover letters need to be quite strategic and targeted for each employer.”
While most students are clear about their preferred employers some of you may not make a final decision about your preferred areas of practice until you are close to completing or have completed your final placement
Then it is a matter of completing your research about the job and employer and pulling it all together in a cover letter that communicates clearly and concisely to the NETP coordinators around the country why they should employ you.
“It can take a good two or three hours to just write a letter to one employer,” says Campbell. And he encourages you to write individual cover letters to each of your up to three prospective employers.
Time for proofing and revising also needed
You also need to build in time for your resume and cover letters to be proofed to ensure there are no spelling or grammatical errors that could put your potential employer off.
“Students are encouraged to get their resume and cover letters proofed and revised by their friends, colleagues or members of their whānau u as well – and that does take time.”
Campbell acknowledges finding that time can be challenging as you juggle working shifts in your final clinical placement and prepare for upcoming exams.
You also need to approach and ask a clinical tutor and a nursing preceptor to be your referee and complete the referee report within the four-week application timeframe.
This can one of the most stressful parts of the process and Campbell says you need to pay attention when inputting their referee details as sometimes students make mistakes –like typing in incorrect email addresses for referees.
For many of you ACE is your first formal job application and sometimes it is not until undertaking a big application like ACE that you fully realise how much time it requires. Campbell says this only dawns on some students when they are stressing to get their applications to ACE complete on time.
But he adds the vast majority of students successfully lodge their applications in a process that has become increasingly streamlined since getting underway in 2012.
Answers to many of your queries can be found on the ACE Nursing website and guidance is also available from the ACE contact centre, your nursing tutors and preceptors, your polytechnic or university careers guidance centre and the NETP coordinators.
And take the advice of Quentin Campbell – and allocate yourself sufficient time for preparing and lodging your application – as it just may take longer than you expect.
TIPS
- The application timeframe is tight and at a busy time for many students
- So allocate yourself a generous amount of time to prepare and complete your application documentation (particularly CV and cover letters)
- A single cover letter can take at least two to three hours to write
- It is advised to write a separate cover letter for each of the employers you are applying to
- Answers to many of your queries can be found on the ACE Nursing website (see below) and the ACE contact centre can help direct you to the appropriate place.
- Guidance and support is also available from your institutions’ careers guidance service, nursing tutors and preceptors and the NETP coordinators.
- Allocate time for your colleagues/ whānau to help proof and revise your cover letters and CV
- Make sure your cover letters and CV are free of spelling or grammatical errors.
- Double check you have correctly entered the contact details – i.e. email addresses – of your referees when lodging your online application.
RESOURCES
ACE Nursing website:
ACE Nursing Facebook page:
https://www.facebook.com/ACENursing/
ACE Nursing guides:
The ACE Applicant Guide 2017 and ACE Nursing CV template can be found here:
https://nursing.acenz.net.nz/content/ACE Resources
What should I include in a cover letter?
Check out advice on cover letters and other application tips in the ACE Nursing website’s Frequently Asked Questions (FAQ) section:
]]>The leaders said high vacancies were not new to the mental health sector but there had been an increase in the demand and complexity of acute mental health clients who often also face housing, addiction and other issues impacting on their wellbeing.
Nursing was investing in growing ‘its own’ through the new entry to specialist practice programmes but leaders believed more early intervention support was also needed in the wider primary health and social services sector to help reduce demand for acute mental health services.
Elaine Wogan, chair of the national Directors of Mental Health Nursing group, said it was obviously of concern when there were high vacancies as that challenged the affected services. She said there had also been a significant increase in demand for services. “Certainly nurses are tired and feel a little overwhelmed at times because we have over-occupancies in our inpatient units – though that ebbs and flows,” said Wogan.
Gina Soanes, chair of the New Zealand Nurses Organisation’s Mental Health Section, said members were feeling pressured – particularly in the acute mental health sector – not only by the vacancies but the flow-on effect of lack of back-up staff to fill-in for nurses when they are sick. “There are a lot of nurses who don’t take sick leave because there are not enough people to cover them but (eventually) get sicker or there is pressure on their families as well.” She said it was also hard to get job satisfaction when there are so many vacancies and nurses were stretched to deliver services. And even if all vacancies were filled the staffing numbers might still not be enough to meet the level of demand, believed Soanes.
Anne Brebner, chair of the College of Mental Health Nurses, cautioned people from over-reacting to the vacancy statistics. She said nearly 100 nursing vacancies spread over the 19 DHB acute inpatient mental health units across the country was not unusual or something the sector was unaware of. “We’re constantly wanting to address recruitment.”
Health Minister Jonathan Coleman said in May that over the past decade demand for secondary mental health and addiction services had increased from around 96,000 people to almost 168,000 – a 75 per cent increase.
Canterbury DHB, according to the figures reported by RNZ, had the highest acute inpatient nursing vacancies, about 30, as the region responds to unprecedented growth in demand for specialist mental health services since the Canterbury quakes.*
The next highest nursing vacancy numbers, according to the data presented to Radio New Zealand were in Auckland, Northland and Counties Manukau DHBs. The highest proportion of CAT team vacancies were in Capital & Coast and Tairawhiti DHBs. While the worst hit with psychiatrist shortages were Tairawhiti, Hawke’s Bay and Counties Manukau.
Brebner said the mental health sector was struggling to recruit nurses in particularly the biggest cities, as DHBs in smaller centres with lower house prices and rents could offer the same salaries as centres like Auckland.
Wogan, who is the mental health nursing leader at Bay of Plenty DHB, agreed that the reality was that the affordability of living in the Auckland area, and perhaps Canterbury, would impact on recruitment to those DHBs.
Brebner, who is also Clinical Nurse Director- Mental Health and Addictions for Counties Manukau Health, said the DHB’s mental health nurse vacancies were running at 8-9 per cent, which was similar to recent years. She said Counties had responded by increasing the number of new graduates it had taken on into its NESP (new entry to specialist practice) programme, which had been above its funded allocation.
She said the College was also aware of issues around the ageing mental health nursing workforce and with the national directors of nursing and Te Pou had been looking into how to support older nurses who want to stay in the paid workforce including looking at flexible rostering and making best use of experienced staff’s mentoring and supervision skills.
“The College is also trying to grow the nurse practitioner workforce in mental health services across the country to bridge that very high end acute caseload work to support the medical staff with some of their shortages.”
All the leaders believed that the current policy push to more early intervention and improved access to primary health and social services sector was important to help reduce the number of people requiring specialist acute mental health services. Wogan and Soanes said social issues like housing, p-addiction and low incomes were impacting on people’s physical and mental health and patients requiring services from acute mental health teams has increasingly high and complex needs.
“The demand for MH and addiction services needs to sit across the whole of the health journey and the wider health workforce,” said Wogan. “Not just in our hospitals it needs to be in our primary health settings..and working in partnership with the NGOs and upskilling some of our workforce.
Brebner said the College had put a lot of time and energy into its mental health credentialing programme to support practice nurses develop their knowledge and skills in working with people presenting with mental health-related issues.
“There’s an opportunity to maybe do more of that to ease and address the issues much, much earlier so they are not developing into needing acute care.”
*In February the DHB reported that a 39 per cent increase in adult specialist mental health presentations saw its mental health teams seeing 700 more clients each month than before the quakes. The Press reported in March that the number of nurses working in specialist mental health services had increased by about 10 per cent since 2012 to around 550 FTE (full time equivalents) last year.
]]>The DHB late last week announced its new leadership and management structure that includes 11 nursing leadership roles being disestablished, to be replaced with seven. It also changes reporting lines for nurses.
In its initial consultation document the DHB was proposing disestablishing 13 nursing leadership positions and replacing them with a chief nursing and midwifery officer and three other senior nursing leadership positions.
But chief executive Chris Fleming said the proposed nursing changes raised the greatest concern including 141 submissions of which 136 opposed the proposed changes (that did away with dedicated nursing directors for areas like medical and surgical services and a number of senior nurse management roles). He said a major theme of the submissions was the value of nurse managers and the roles they played in quality improvement, culture and patient safety.
After discussions with the executive director of nursing and midwifery, Leanne Samuel, and the New Zealand Nurses Organisation he decided to review the nursing proposal leading to the final decision announced at 5pm on June 30.
The positions being disestablished include Samuel’s executive director of nursing and midwifery position which is to be replaced with a chief nursing and midwifery officer role. The new role will split off operational responsibility for nursing and midwifery staff and change the reporting line for the new tier of nursing leaders. But the role will still be part of the executive leadership team and report directly to the CEO
Currently five nursing directors and the midwifery director report directly to Samuel and 715 fulltime equivalent (FTE) nurses. This will change to four nurse leadership roles reporting directly to the chief nursing officer and 14 indirect reports
Most charge nurse managers will report to the five directors of nursing who will report to the operations manager or executive director of the section. Most of the new inhouse positions will be internally advertised this month. Across the DHB 55 leadership positions are being disestablished and replaced with 42.
NEW NURSING ROLES ESTABLISHED (to replace 11 disestablished roles)
- Chief Nursing and Midwifery Officer
- Director of Nursing Southland
- Director of Nursing Surgical, Dunedin
- Director of Nursing Medical, Women & Children, Dunedin
- Director of Nursing Strategy, Primary & Community, DHB wide
- Associate Director of Nursing Southland
- CNM Perioperative, Southland
NAME CHANGES ONLY
- Director of Midwifery
- Director of Nursing Mental Health & Addictions and Intellectual Disability
- Associate Director of Nursing Surgical Dunedin – Perioperative & ICU
- Associate Director of Nursing Medicine – Southern Blood & Cancer