This backs ongoing calls by the national nursing organisations for 100 per cent placement of new graduates in new graduate programmes – a goal they had set to be met by this year.
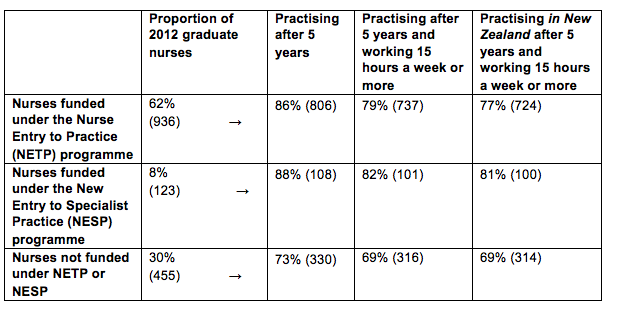
The Ministry of Health analysis found that 86 per cent (806) of the 2012 nurse graduates who gained a place in a government-subsidised NETP (Nurse Entry to Practice) programmes were still in nursing five years on.
The proportion was even higher for mental health nurses with 88 per cent of the 123 new grads signed up to a specialist mental health NESP (New Entry to Specialist Practice) Programme) still having valid annual practising certificates (APC) five years later.
In comparison just 73 per cent (330) of the 455 new graduates who failed to gain a place in a NETP or NESP programme still had an APC in 2017. Overall 1244 (82%) of the 1514 nurse graduates registered in 2012 were still in nursing five years later. (See table below)
Chief Nurse Jane O’Malley said the higher proportion of new graduates still nursing if they had started their careers in a funded new graduate programme was “telling” and showed the importance of the programmes for nursing retention.
In 2013 the National Nursing Organisations – including the New Zealand Nurses Organisation and College of Nurses Aotearoa – called for full utilisation of all NETP funding to support the goal of 100 per cent employment of new graduates by 2018. Government funding is potentially available to subsidise 1300 NETP and about 125 NESP places but lack of vacancies and tight budgets – particularly at district health boards – means only all the NESP funding is fully utilised.
New graduate nurses employed under a year-long NETP programme must receive clinical preceptor support for the duration of the programme and the equivalent of 12 study days with the aim of new nurses starting their career “well supported, safe, skilled and confident in their clinical practice”.
The analysis of the 2012 new graduate cohort – that uses data from the ACE new graduate placement and Nursing Council of New Zealand annual practising certificate data – also showed the vast majority of the new nurses still holding APCs were practising for more than 15 hours a week. (NB nurses practising for less than 15 hours a week but still with valid APCs may be on parental leave, travelling overseas or between jobs.)
The APC data indicated that just over a dozen nurses with valid New Zealand APCs were currently practising overseas. (Retaining an NZ APC indicates that they may only be working overseas for a limited amount of time and/or wanted to retain the option of returning to New Zealand to nurse.)
]]>
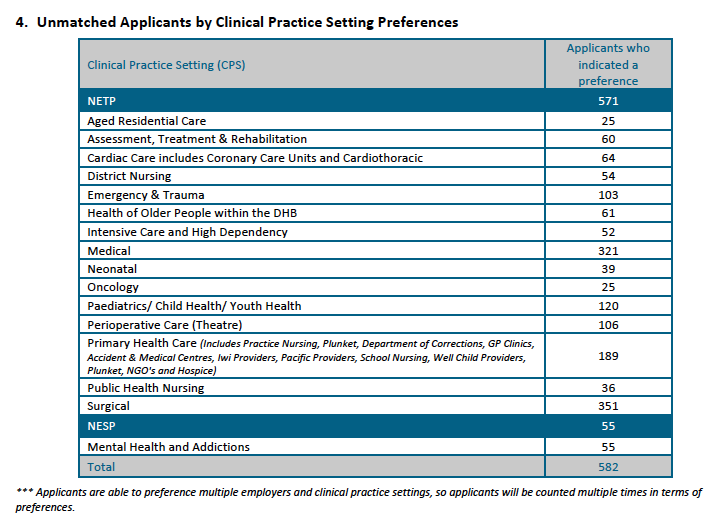
Overall 582 (43 per cent) of the 1389 applicants found out on November 22 last year that they were unsuccessful in the first job match. While most of the unsuccessful applicants were seeking surgical or medical nursing positions, the latest ACE report shows a high proportion of graduates seeking mental health and addictions, aged residential care and primary health care roles were also unsuccessful.
Hilary Graham-Smith, professional services associate manager for the New Zealand Nurses Organisation, said yesterday that hundreds of graduates missing out on jobs was unacceptable considering the national nursing workforce goal was 100 per cent placement by 2018.
The ACE Nursing Algorithmic Match Report provides a breakdown of the 913 jobs on offer and the 775 new graduates matched with jobs on November 10 in the end-of-year round of the ACE new graduate nurse job-matching process. In all, 57 per cent of the 1389 applicants found out on November 22 that they had been offered positions on Nurse Entry to Practice (NETP) and Nurse Entry to Specialist Practice (NESP) programmes. At least 138 positions were still to be filled as at November 10 and historically more graduates are also offered jobs over the summer break as vacancies arise leading up to NETP and NESP programmes getting underway in late January/early February this year.
Graham-Smith said the overall trend in new graduate jobs for nurses showed no significant increase. “This is not the case in medicine: every new graduate doctor has a place on an entry programme. This speaks to the chronic under-investment in nursing and a complete lack of progress on guaranteeing all new graduates of a place on a programme by 2018,” she said.
She said Health Workforce New Zealand head Des Gorman has called it a “perfect storm” as nursing has gone through a long period of under recruitment and training. “This matches our research on nursing employment. We have an aging workforce and over-50s leaving. We are simply not attracting, training or retaining enough nurses to future-proof our healthcare services,” she said.
Concern was expressed last year about shortages and high vacancies for acute mental health nursing positions. The ACE match report shows that 55 of the 210 applicants who expressed interest in the NESP programmes for mental health and addiction nurses were unsuccessful.
In addition, 25 of the 39 nurses who indicated a preference for aged residential care and 189 of the 359 who were keen on primary healthcare positions (which include practice nursing, prison nursing, Plunket and hospice positions) were unsuccessful in the first job round.
The DHBs in which it was hardest to get jobs (i.e. which turned away the highest proportion of applicants who had put that DHB down as their first preference) included Hutt Valley, Mid-Central, Capital & Coast, Waikato, and Auckland, which accepted between 28 to 42 per cent per cent of the first-preference applicants (see table at bottom of article for the number of jobs on offer).
Ethnicity and second-time-around job rates
The percentage of Māori and Pacific nurse graduates offered jobs on November 10 was again slightly higher than the average job success rate at 70 per cent (145 of 206 applicants) and 63 per cent (54 of 85 applicants) respectively, compared with 57 per cent for all applicants.
Asian applicants were once again the least successful in obtaining job offers, with just 39 per cent (86) of the 220 applicants being offered a job in the first round. The job rate for the ‘other’ ethnicity category (largely Pākehā/European) was the same as for all applicants – 57 per cent – with 490 of the 846 applicants being successful.
The vast majority of the November applicants were first-time-round applicants and 60.5 per cent of those applicants were successful. Just over 35 per cent of the 115 second-time-round applicants were successful and 26 per cent of the 49 applicants applying for a third time or more.
The ACE Nursing Intake Summary Report was prepared by the agency TAS (formerly known as DHB Shared Services), which owns ACE Nursing on behalf of the 20 DHBs.
The next ACE report is not due until after the National Talent Pool, from which DHBs can employ unmatched new graduate applicants, closes in late June.
Report author Kamini Pather said there was a lot of dynamic change to ACE daily statistics as applicants get offered jobs, withdraw from the talent pool for other reasons or change their preferences. This meant there were only two points in the recruitment cycle where stable and reliable data could be extracted. Those were at the time of the electronic match (November 10) and once the National Talent Pool and end-of-year intake closes, which is about seven months later in late June.
| Employer | Positions submitted to ACE Nursing for End of Year Match | Total Applicants Matched to Employer (as at Nov 10 2017)
|
| Auckland DHB | 107 | 79 |
| Bay of Plenty DHB | 49 | 49 |
| Canterbury DHB | 112 | 100 |
| Capital & Coast DHB | 65 | 56 |
| Counties Manukau DHB | 97 | 80 |
| Hawke’s Bay DHB | 32 | 29 |
| Hutt Valley DHB | 14 | 14 |
| Lakes DHB | 17 | 17 |
| MidCentral DHB | 19 | 14 |
| Nelson Marlborough DHB | 37 | 37 |
| Northland DHB | 24 | 22 |
| South Canterbury DHB | 15 | 13 |
| Southern DHB | 58 | 53 |
| Tairawhiti DHB | 10 | 10 |
| Taranaki DHB | 23 | 21 |
| Waikato DHB | 94 | 66 |
| Wairarapa DHB | 4 | 4 |
| Waitemata DHB | 97 | 78 |
| West Coast DHB | 5 | 4 |
| Whanganui DHB | 18 | 18 |
| Southern Cross Hospitals – Auckland | 7 | 3 |
| Southern Cross Hospitals – Midland (Waikato & BoP) | 3 | 3 |
| Southern Cross Hospitals – Southern (Christchurch) | 6 | 5 |
| Total | 913 | 775 |
]]>
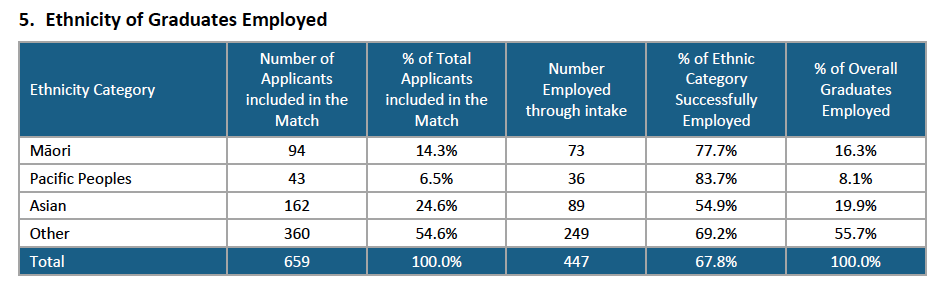
The ACE Nursing Intake Summary Report** for the mid-year intake showed that 447 – just short of 68 per cent of the 659 applicants – received a job offer for a new graduate programme place between July and late October via the ACE job-match process.
When the mid-year pool closed on October 27 there were 190 (28.8%) left in the pool who were still seeking supported new graduate jobs – over a hundred less than the same time last year.
This was the lowest percentage of the mid-year intake still job-hunting into the spring since ACE records began in mid-2013 – and just over a hundred less than the same time last year, when 43 per cent of mid-year applicants were still job-hunting in the spring.
The 51 nurses taken on by mental health and addiction providers for NESP [new entry to specialist practice – mental health and addictions] programmes contributed. The improved mid-year employment rate was also reflected in the findings of the annual mid-year graduate survey undertaken by NETS (Nurse Education in the Tertiary Sector).
According to the ACE report Pacific nurse graduates were proportionately the most successful in getting a job through ACE with 83.7 per cent of the 43 applicants being employed. The next most successful were Māori graduates with 77.7% of the 94 applicants being matched with a job.
The “other” ethnicity category – which includes New Zealanders of European descent – made up just over half of the applicants – 360 (54.6%) and had a job success rate of 69.2%, which was just above the overall job success rate of 67.8 per cent*. Kiwi nurse graduates of Asian ethnicity made up 162 (24.2%) of applicants and had a 54.9% per cent job success rate – the lowest of the four ethnic groupings. (NB to be eligible to apply for a funded NETP [nursing entry to practice] or NESP [new entry to specialist practice – mental health] position through ACE you need to be a New Zealand citizen or hold a permanent/returning resident visa.)
In November 2015 the Health Workforce New Zealand’s (HWNZ) Nursing Governance Taskforce for Nursing set a date of 2028 to meet a goal of significantly increasing the number of Māori nurses so as to better match the proportion of Māori in the population, with the aim of improving access to care and the quality of care for Māori. ACE statistics for the end of 2015 showed 54 per cent of Māori graduates were known to be employed, compared to 50 per cent of non-Maori and 53 per cent of Pacific applicants.
By mid-2016 the Governance Taskforce had consulted and endorsed ‘levers’ to help meet the goal including supporting all Māori new graduates into employment, building on current initiatives to promote nursing careers, and building Mâori faculty at universities and other providers.
The mid-year intake analysis indicate that the push may be paying off but the director of the Wānanga based kaupapa Māori nursing degree, Ngaira Harker, has expressed disappointment at the intial job offers for its first graduate cohort of 19 nurses who are part of the latest end-of-year ACE intake. At the end of November nine had jobs (just under half) which was a lower job rate than the 57 per cent of total applicants who had been offered jobs in the same time period, according to early ACE stats for this latest job match round.
Auckland biggest source of jobs
The cost of living in Auckland didn’t seem to put off new graduates seeking work for the three Auckland district health boards.
Auckland DHB had the highest number of applicants putting it as their first preference (118) and had 312 applicants in total expressing a preference for Auckland as their first, second or third preference. Waitemata DHB was the first, second or third preference of 229 applicants and Counties-Manukau had 200 applicants.
In all there were 260 applicants in the mid-year intake (just under 40 per cent of total applicants) who were graduates from the five nursing schools based in Auckland. The three Auckland DHBs between them took on 199 new graduates (Auckland DHB 87 and the other two 56 each) which was the equivalent of 44.5 per cent of the total jobs on offer nationwide.
The other two largest DHBs, Canterbury and Waikato – also got high interest with 108 graduates putting Waikato as their first preference and 106 putting Canterbury.
Canterbury DHB employed the highest number of new graduates in the country, 91, and Waikato employed 56.
*ACE Nursing mid-year job match round statistics
- 659 applicants took part in the ACE mid-year job match (461 were first time applicants, 169 second-time applicants and 29 were applying for their third round or more.)
- 389 jobs were initially offered by employers (338 NETP and 51 NESP)
- 327 applicants in July were electronically matched and a further 26 manually matched with jobs.
- 346 accepted the job offers (seven applicants failed state finals or declined job offers)
- 101 of the remaining 306 unmatched applicants were offered jobs before the ACE national talent pool closed on October 27.
- 447 (67.8%) of ACE applicants in total were successfully matched with a job.
- That left 190 (28.8%) of applicants still seeking a NETP or NESP placement as at October 27 and a further 22 (3.4%) of applicants had declined offers, failed state exams or withdrawn from the pool.
**The ACE Nursing Intake Summary Report was prepared by agency TAS (formerly known as DHB Shared Services) which owns ACE Nursing on behalf of the 20 DHBs.
NB: This article was corrected on December 22 to clarify that the report was released by TAS rather than the Ministry of Health.
]]>But there were 583 new graduate applicants without job offers vying for those remaining 139 positions. So many new nurses will once again start the summer job-hunting and hoping more positions will open up over the Christmas/New Year break.
The Ministry of Health this week released initial data on the 2017 ACE Nursing end-of-year job ‘match’ between the 1357 new graduate nurses who applied and the 901 positions on NETP (Nurse Entry to Practice) and NESP (new entry to specialist practice, mental health and addictions) programmes being offered via the 20 district health boards and Southern Cross.
In the first round in mid-November 774 applicants (57 per cent) were matched and were sent job offers on November 22, leaving 139 positions still to be filled by the remaining 583 applicants in the talent pool.
The proportion of graduates matched with jobs by mid-November appears to be slightly up on last year. Statistics released on December 9 last year for the 2016 round showed 779 new grads had jobs (54 per cent of applicants) but that figure included 16 applicants who secured jobs after the initial mid-November match and 13 applicants known to have got non-NETP or NESP positions. The number of applicants in 2016 was the highest ever with 1455 initial applicants of which 1434 took part in the job match.
Further information on the latest round will be made available in mid-December including which clinical settings the new nurses have been offered jobs in and how many graduates have accepted the initial job offers and how many jobs were still to be filled from the remaining talent pool.
The Ministry of Health says data trends from previous end-of-year new graduate recruitment rounds have followed a similar pattern with about 50 per cent of graduates gaining employment before they know the outcome of the Nursing Council State exam and that almost all (96-98%) graduates applying though ACE will be employed within 12 months. But a number of these will be employed outside of the government-subsidised and mentored NETP and NESP programmes – including in residential aged care – which has prompted continued calls from nursing organisations for all graduates to be offered new graduate programme places.
New graduate Nov ACE job trends
| Year | Total applicants* | First time applicants | Total number of jobs offered** | Total number of applicants successful |
| 2012 | 1239 | NA | 730 | 58.9% |
| 2013 | 1337 | NA | 605 | 45.2% |
| 2014 | 1481 | 1260 | 778 | 52.5% |
| 2015 | 1451 | 1245 | 735 | 50.6% |
| 2016
2017 |
1455
1357 |
1274
NA |
779
774* (*filled as at Nov 10 of 913 positions available)
|
53.5%
57.0%
|
*Number of applicants can drop by the time job offers are made in mid-November as graduates either get jobs with other employers or withdraw for other reasons. From 2014 onwards eligibility for applying to ACE nursing was extended so new graduates could apply for NETP/NESP positions for up to two years (i.e. up to four times) after passing state finals.
**The cut-off date for supplying job offer data can vary slightly from year to year from – so sometimes includes additional jobs offered in late Nov/early December. Employers keep offering jobs over the summer so the number who actually start NETP programmes in the New Year is always higher.
NA = not available
]]>So stated the 1998 Ministerial Taskforce on Nursing. The Taskforce report also noted many acute hospitals expected nursing graduates to “immediately take up a high workload and a high level of responsibility with little structured help or support”.
It’s been 10 years since the government gave the green light to funding new graduate programmes, bringing in the first nationally consistent clinical training support for novice nurses.
At the time, support for new graduates in their first year of practice varied considerably across the country with some fortunate new graduates securing a place in formal new graduate programmes and others, like the less fortunate casual pool nurses, being expected to be work-ready in any setting.
The gold standard then was the already long-established new graduate programme for mental health nurses (now known as the NESP or new entry to specialist practice programme). The Taskforce recommended NESP be the template for a national framework of funded new graduate programmes to support this “vital time in the development of a truly professional and effective nurse”.
After a pilot in 2002 and a positive evaluation report in 2004, the government in July 2005 finally announced funding for a national framework of nursing entry to practice programmes (NETP).
So in mid-2006 the first three district health boards to gain Nursing Council accreditation for their NETP programmes were given a subsidy of $6,000 per graduate to deliver the course – roughly 50 per cent of the estimated cost. The rest of the DHBs came on board in 2007 and in 2009 the first NETP places were offered in primary health and residential aged care.
Fluctuating supply and demand for NETP places
For many of the early years of NETP there were more funded places available than were ever filled, with a number of DHBs struggling to attract new graduates in a buoyant job market.
But this reversed when the global financial crisis saw nursing turnover stagnate and DHB budgets tighten, at the same time as record numbers were graduating from the country’s nursing schools in readiness to replace the country’s ageing nursing workforce.
It was a perfect storm that saw NETP numbers fall and plateau in 2010 and 2011 (see table) and then start to steadily climb, but not fast enough to match the growing graduate cohorts. Faced with keen new graduates struggling to find work – and the added fear they could be lost to the profession, which would ultimately need them to replace retiring baby boomers – the New Zealand Nurses Organisation (NZNO) last year launched a petition calling for the government to fund an NETP place for every graduate.
The petition reached 8,000 signatures and the then health minister, Tony Ryall, responded by announcing 1,300 NETP places would be funded in 2015. Unfortunately, with nearly 1,800 new graduates registered last year, this falls far short of NZNO’s expectations. Also, whether the sector will be able to step up and employ 300 more nurses than last year (see table) to fill those extra NETP places is yet to be seen.
Improved data is now available on graduate trends through the central clearinghouse for NETP and NESP applications known as ACE, which was first used for the February 2013 NETP intake. The February 2015 ACE round saw an increase in new graduates in NETP jobs and also saw places in the mental health NESP programmes swell from 152 last year to 175 this year. And for the first time NETP funding has been allocated to new graduates employed at private surgical hospital provider Southern Cross (see sidebar).
NETP: a year for clinical consolidation and/or postgraduate study?
“I don’t think anybody would argue that the NETP programme has been a tremendous asset to establishing people’s first year of practice in a safer way then we used to do,” says Professor Jenny Carryer, executive director of the College of Nurses.
“But there are still issues around the fact that we are not funded for every single graduate and so a number of graduates miss out on the NETP programme, therefore can fall between the cracks,” says Carryer.
While only a handful of DHBs at the outset included postgraduate papers as part of their NETP programme, this has expanded over the years until only a handful now do not. Some DHBs have taken this a step further and are offering top graduates an honours programme in their second year, with the option of progressing into studying for a health sciences doctorate.
Carryer, for one, sits in the camp that believes NETP should be a year focused on the consolidation of clinical skills. “It is a year they [new graduates] are under enormous pressure to think on their feet, time manage and take responsibility for decision-making – all of those first-year learning challenges. And personally I don’t think we should distract them with a postgraduate paper that year.” Also, graduates in their first year of practice usually haven’t yet decided on their likely career path or specialty.
Sitting in the other camp is associate professor Judy Kilpatrick, head of The University of Auckland nursing school, which offers postgraduate papers in partnership with many DHBs’ NETP programmes.
“What we actually found was that graduates were doing some quite high-level things in that first year and postgraduate study was a perfect way to give credit and shape up their thinking.” She said the paper involved a high level of clinical assessment but formal study did not commence until the second semester of the NETP year to give graduates a chance to adjust to working life.
“I think that postgrad study firstly helps retain the graduates; secondly, they are able to get new knowledge – at a sharper and higher level than undergraduate – that they can apply in the clinical area; and lastly, by the end of the first year they are already cementing themselves in the pathway of where they want to go.” She says rather than being burnt out, the graduates all complete and many will go on to pursue further postgraduate study (though quite a few take a break after completing their postgraduate certificate and look around before resuming study at the next level).
Sue Hayward, director of nursing for Waikato DHB, which offers the honours programme to leading second-year nurses and now has two recent graduates on the doctoral path, also believes postgraduate study in the NETP year consolidates what graduates have learnt in their undergraduate degree.
She says the Midlands region of DHBs have negotiated for graduates then to have a longer gap, if they wish, before they do the second paper of their postgrad cert but most have completed their certificate within three years. “It’s not arduous – though it’s not easy,” says Hayward. And retention, even taking into account the current economic environment, was very good, with 96 per cent of NETP graduates staying on and going into permanent positions.
Dr Kathy Holloway, national chair of nurse educator group NETS, was part of a team that evaluated the first three years of NETP and found the supported first year of practice programmes was enhancing trainees’ confidence and competence.
She says DHBs had always done some form of new graduate programme but they were very variable across the country and there needed to be some consistency and structure, which national funding enabled it to have. And expanding the scheme into primary health care, aged care facilities, some non-governmental organisations and some private surgical hospitals meant it could support graduates entering the wider nursing workforce.
“But we still have the goal of 100 per cent employment of nurse graduates into an NETP position if they seek one.”
Southern Cross joins NETP
Southern Cross this year became the first private surgical hospital group to get NETP government subsidies for its new graduates
Carey Campbell, chief nurse advisor for Southern Cross Hospitals, said Southern Cross first started working towards gaining NETP funding in 2010 but at the time Health Workforce New Zealand (HWNZ) specifications didn’t allow government funding for new graduates employed by private surgical hospitals.
But she says by 2013/14 the country’s private surgical hospitals were employing about 50 new graduates (25 of those by Southern Cross). “This was a significant contribution to the nursing workforce – the number being larger than many DHBs.”
Campbell said sharing this information with HWNZ and the Ministry of Health’s Office of the Chief Nurse at the same time as there was ministerial pressure over employing new graduates “certainly helped our cause”.
HWNZ spokesman Ruth Anderson said it considered Southern Cross’s application last year as part of its commitment to increase the number of new graduates employed in quality entry to practice programmes. It also followed the government’s July 2015 announcement to fund up to 200 additional new graduate places in 2015.
“HWNZ has a role to ensure the sustainability of all parts of New Zealand’s health workforce,” said Anderson. “To fulfill this role, funding support for training in both the public and private sectors must be considered.”
As a result, HWNZ agreed in October 2014 to fund Southern Cross for up to 25 new NETP new graduates in 2015 ($7,200 per graduate) dependent upon Southern Cross’s NETP programme getting Nursing Council approval.
Campbell said Southern Cross gained Nursing Council approval in April and currently has 20 new graduate RNs employed across the country, with 17 funded through NETP. Two further NETP places will be available in the September intake, making a total of 19 NETP this year.
For the first time, Southern Cross will also be added as an employer option for new graduates applying through the Advanced Choice of Employment (ACE) recruitment clearinghouse for the 2016 NETP intake. The number of NETP places Southern Cross will be funded for in 2016 is still under discussion and HWNZ says it also needs to consider existing training funding commitments to district health boards.
NETP places filled
2006: 174
2007: 710
2008: 813
2009: 886
2010: 840
2011: 835
2012: 911
2013: 933
2014: 1000
2015: 777 (to date) – funding available for 1300*)
*NB The funded places for NETP have always exceeded the number actually filled. In the early days of NETP some DHBs struggled to attract new graduates into their programmes and then in more recent years low nurse turnover and tight budgets has meant more demand for places than DHBs were able to deliver.
NETP specifications
- A maximum of two clinical placements/rotations within the maximum 12-month programme.
- Clinical preceptor support throughout the duration of the programme (sharing clinical caseload for six weeks in total).
- The equivalent of 12 group learning/study days (including any postgraduate papers).
- A sub-contract between the parent DHB and any other employer, i.e. general practice or residential aged care facility.
- Health Workforce New Zealand funds $7,200 per graduate towards six-week clinical caseload sharing by preceptor, 12 days release time for study days and 16 hours training for preceptors.
- Aged residential care providers meeting certain training criteria can receive an additional $12,800 to cover extra preceptorship and supernumerary release time.
NETP pioneer inspired to nurture today’s new nurses
Sharon Fisher was not new to her first ward but still recalls those first few weeks as a ‘real’ nurse as “absolutely terrifying”.
The mature student and mother of two had had a student placement at the Waitakere Hospital medical ward that became her nursing home as a new graduate nurse in Waitemata DHB’s first official NETP cohort (also one of the country’s first) back in 2006. The ward was familiar and friendly but being a new nurse was still testing to the nerves.
“I can recall around week four doing a blood pressure on a patient and it was something ridiculous like 80/60 when I knew that 120/80 was normal,” recalls Fisher with a laugh.
“I wasn’t panicked as such but I was certainly perturbed and can just remember the clinical coach being on the floor at that stage and calming me down by making me aware that you look at the patient as a whole, rather than as a set of numbers. So when I took that into account I realised she was a tiny little dot of an old lady… and I recall feeling really, really supported by my ward staff and the NETP people.”
Fisher had applied to both Auckland and Waitemata DHBs and been accepted by both but chose Waitakere as she had enjoyed her placement and lived ‘out west’.
But another factor was Waitemata’s NETP at that stage did not include a postgraduate paper and after three years of study with two preschoolers, she didn’t want to do any more study for a while. “I really felt that a year of just learning to be a nurse – without the pressure of more study [was what she wanted].” (Though she has since done the assessment paper now offered in the NETP year and thinks it may not have been as hideous as she had feared as a new graduate.)
Looking back, Fisher can recall near the end of her NETP year an incident when she had the confidence to test her nursing wings. “I had a patient who was dying in a little windowless treatment room and I had the opportunity to move her into a single room with a view over our little pond – so I did.
“Our charge nurse questioned me, as the patient died within hours, about the cost of the moving, extra cleaning etc – and I can recall feeling very much that I was able to justify why I’d done it. I really felt that for the family to have their family member die in a room with a nice view and some sunshine rather than a poky internal room was an important part of that patient’s death. I thought it was the ethical, right thing to do … and I certainly wouldn’t have done that at the beginning of my new grad year.”
Fisher went on to become a district nurse, still based at Waitakere Hospital. She completed her postgraduate diploma and has started her Master of Health Science research thesis looking at new graduates’ interest in placements with older adults.
She herself also became a preceptor and rece02ntly successfully applied for a clinical coach position within the NETP programme, which she sees as playing a vital role in nursing.
“I think if we can get in and shape our new grads at the beginning and give them an experience like I had – I’m still nursing 10 years down the track and I’m still at Waitakere.” She says being able to spend time with fellow new graduates in the same position as herself made a “huge impact” as that year can be “overwhelming” and she definitely sees herself long-term working as a nurse educator to help nurture new nurses.
Supportive new grad year sealed love for ED nursing
Lola Brownlee’s new grad year in ED was so positive she is still there a decade later.
Another of Waitemata DHB’s first cohort of NETP graduates, she started in North Shore Hospital’s emergency department (ED) in 2006. She has now completed her clinical master’s in emergency medicine and is one of the ED’s team of clinical charge nurses.
The former bookkeeper and mother-turned-nurse recalls being excited just being on the floor doing what she had chosen to be her new career – nursing, though it was also quite daunting coming from nursing school straight to ED as you initially thought you didn’t know anything. “But you quickly learn, with support, to trust what you’ve learnt and to trust the people around you … and with NETP you’ve got somebody you can trust to ask the silly questions to make sure everything is okay.”
She says her pioneering ED NETP programme may not have included postgraduate papers but did include intense learning of the ED training manuals for each area and training in areas like cardiac assessment skills and resuscitation. “I think to do postgrad study in the first year in ED would have been too much because we had so much learning to do on the floor that year but they’ve revamped our ED programme and now they start postgrad study in the second semester. I think some new grads find it difficult to try and learn what they need for working on the ED floor, as well as postgrad study.”
Brownlee thinks ED is possibly slightly different from nursing in other acute areas. Just consolidating newly learnt skills in the first year could be a good thing, she says, then starting postgrad study in the second year when nurses better “know what they don’t know”.
“I think the support I got from the coaches in the new grad programme was really amazing. So I never felt scared – though there were times I felt challenged… like the first time you see a death.”
Brownlee says in time, and with support, you can tell from the data and your observations that the patient in front of you is not just sick but really sick and you realise you are really nursing.
“It boosts your confidence that you’ve developed that critical thinking where you can tie things together and when you go to the doctor there is a reaction and they start trusting you as a nurse – it’s quite exciting.”