It warned that New Zealand was “quickly becoming a society divided by the ownership of housing and its related wealth”.
It also showed home ownership had slumped dramatically since the 1980s – especially among Pacific and Maori people – and Auckland’s housing problem was created by a mix of population growth, partly fuelled by migration, and the construction and land development sectors “hindering” housing affordability.
It also pointed to a potential time bomb in the impact on housing affordability on the elderly, finding the proportion of older people who were living in mortgage-free homes had dropped from 86 per cent to 72 per cent since the 1980s.
The housing report was authored by economist Shamubeel Eaqub, University of Otago Professor of Public Health Philippa Howden-Chapman and the Salvation Army’s Allan Johnson.
‘Sobering’ reading
Twyford said it was “sobering”.
“It paints a sobering picture of the devastating impacts of the housing crisis, particularly on children. Homelessness, transience and substandard housing have had a lasting and sometimes even deadly effect on our youngest.”
It included discussion of the “hidden homeless” population that is not officially monitored or recorded.
However, community emergency housing providers report they are at full capacity, and their data from last year indicates that for every 10 homeless people that approach them, eight to nine are turned away.
The report shows homelessness was worse than previously thought and that 80 per cent of homeless people turning up to community emergency housing providers in the last year were turned away.
It brings together figures across a number of areas including homelessness, the rental market, housing affordability – including the rising costs relative to wage increases – and housing supply nationwide, with a specific focus on Auckland.
The report warns of a burgeoning “floating population” – people without safe and secure housing, including in temporary housing, sharing with another household, or living in uninhabitable places.
Greater awareness of the issue, along with more information campaigns about where to get help, is expected to lead to reported homelessness getting worse.
The report is intended as analysis of the housing issue, and is not expected to make any recommendations for action.
One indication of the extent of the crisis in the report is an extra 2000 pensioners receiving the accommodation supplement last year.
‘Pipeline of homelessness’
Alan Johnson of the Salvation Army was one of the report’s authors. He warned that homelessness would get worse before it got better.
“We believe there’s a pipeline of homelessness still in existence. There will be some time yet before we see the numbers in transitional housing tapering off. We believe it will get worse before it gets better.”
He had looked at housing assistance programmes, homelessness and transitional housing. He said the previous National Government’s reforms in the area of social housing and state housing were “poorly funded and poorly executed”.
“It’s apparent to us that one of the problems we’re had in social housing or state housing areas was that the previous government’s reform agenda was in parts an essential programme in terms of rejuvenation of housing stock, but the reality is it was poorly funded and poorly executed.”
Johnson said reform of the Accommodation Supplement was needed, beyond the increase due mid-year under the Government’s families package as hundreds of thousands were dependent on it.
He said abatements created ”poverty traps” and the current system was arbitrary and could act as a disincentive for people to take on part-time work.
He said there should be a preference for fixed-term tenures, rather than periodic, and those should provide a way to moderate rent increases.
The Tenancy Tribunal was funded from the interest off tenants’ bonds, yet it was landlords who used the Tribunal more. That funding should be used more for tenants’ rights, he said.
Otago University Public Health professor Philippe Howden-Chapman said the numbers of children who did not live in homes owned by their families had grown.
“This has fundamentally major consequences for stability in communities.”
She said in Otago’s “Living in New Zealand” long-term study, those who had not lived in stable housing as a child had faced different consequences than others.
She said little work had been done on the social costs of substandard housing in New Zealand and it was beneficial for the government to be looking at the consequences of housing on the wellbeing of people.
Economist Shamubeel Eaqub has hit out at the Labour Government’s fiscal responsibility rules, saying it was acting as a “straitjacket” on it and debt could be used to reform the housing market.
Eaqub was one of the authors of a housing stocktake commissioned by the Government to help guide housing policy.
Eaqub said investment was needed in infrastructure and housing such as the KiwiBuild programme yet the Government was restricted because of the fiscal responsibility rules.
He said the infrastructure issue could be resolved by “borrowing s***loads of money” and only a “fiscal idiot” would not have been borrowing money in the current climate or over the past decade.
Labour and the Greens both signed up for fiscal responsibility rules requiring the Government to stay in surplus and to gradually reduce government debt relative to GDP to 20 per cent.
Housing report: key points
• Population has outstripped housing growth by 2.1 per cent
• New Zealand has 1.9 million private homes with average of 2.6 people per dwelling • 574,000 households are renting
• Rents for three-bedroom houses rose 25 per cent 2012-17, but wages just 14 per cent
• 32 per cent of rental properties are “poorly maintained”
• 29 per cent of households struggle to afford power bills, spent a large portion on the bill, or felt cold
• Number of children under 15 living in rentals up 65 per cent between 1986 and 2013
• Child asthma estimated to have cost $58.3m in 2013
• Between 1991 and 2013 the proportion of Maori renting privately rose from 41 per cent to 77 per cent and for Pasifika from 27 per cent to 56 per cent.
• “This rise appears to be fuelled by the decrease in state housing stock and changes to policies designed to move people out of state housing.”
• 6128 households needing a state house in December 2017
• One in 100 people homeless in 2017, up from one in 120 in 2006
• For every 10 people approaching emergency housing providers in 2017, eight or nine turned away
Source: A Stocktake of New Zealand’s Housing.
The three public health professionals from the University of Otago say New Zealand’s current emergency plans focus on influenza and have little guidance for emerging infectious diseases, such as the recent Ebola and Zika outbreaks. Also the National health Emergency Plan: Infectious Diseases, developed in response to the SARS epidemic in 2003, was now out of date, leaving the Influenza Pandemic Preparedness Plan 2010 as the core document.
“The Ministry of Health’s ‘Pandemic Planning and Response’ webpage links only to documents regarding influenza,” point out the authors in an article published today in the Australian and New Zealand Journal of Public Health.
“However, preparedness for pandemic influenza does not guarantee preparedness for another emerging infectious disease, as demonstrated by the emergence of blood-borne (Ebola) and vector-borne (Zika) threats in recent years.”
The trio point out that emerging infectious diseases have caused pandemics with the highest death rates in history, including the plague, the influenza of 1918/19, and HIV.
Outbreaks of emerging infectious diseases have also been on the increase since 1940, with many caused by zoonotic diseases (diseases that can be transmitted from animals to people), while at the same time antimicrobial resistance is increasing worldwide in what has been described as a “slow-motion tsunami”.
Recommendations in the article for New Zealand health authorities include:
- implementing an antimicrobial resistance plan (including strengthened collaboration between human and animal health sectors)
- developing laboratory capacity for highly pathogenic organisms (ideally with shared planning and capacity building with Australia to maximise cost-effectiveness)
- developing real time surveillance beyond notifiable diseases and influenza
- developing or adopting a framework to cover prevention, detection and response to a broad range of emerging infectious diseases, especially those with greatest potential to spread in our region
- conducting regular exercises to test plans for emerging infectious diseases other than pandemic influenza (but additional exercises on pandemic influenza are still warranted, e.g. every 5–10 years)
- undertaking regular joint external assessments of IHR (International Health Regulations) core capacities both in New Zealand, and assisting low- and middle-income countries in the Pacific Region to undergo assessments and develop their capacities.
]]>
World Antibiotic Awareness Week 2017 (November 13 to 19) is a World Health Organization global event around one of the most pressing challenges to health care – including the risk of relatively common infections developing resistance to the antibiotics usually used to treat them.
Late last year New Zealand’s Council of Medical Colleges facilitated the local launch of the global Choosing Wisely initiative in partnership with the Health Quality and Safety Commission and Consumer. The initiative – targeted at both health professionals and consumers – aims to avoid unnecessary clinical interventions including inappropriate prescribing of antibiotics.
Dr John Bonning, from the Council’s executive, said a growing number of infections, such as pneumonia, tuberculosis, and gonorrhoea, are becoming harder to treat as the antibiotics used to treat them become less effective. He said as part of the Choosing Wisely campaign the Council worked with Australasian and New Zealand Colleges and specialist societies to develop specific recommendations about antibiotic use.
“These recommendations include situations when antibiotics should not routinely be used – such as for upper respiratory tract infections, the use of topical antibiotics on surgical wounds, and for the treatment of fever in children without a bacterial infection.” (See list of recommendations and links below.)
The Ministry of Health’s Director of Public Health, Dr Caroline McElnay, says New Zealand this year presented its Antimicrobial Resistance Action Plan as part of the commitment to tackling the global challenge.
Michael Baker, spokesperson for the College of Public Health Medicine said it was essential that New Zealand implemented the plan and echoed that antibiotic resistance was a global issue in which New Zealand “absolutely has to play its part”. “We need widespread commitment and leadership from medical, veterinary and agricultural sectors in New Zealand, working together.”
Hilary Graham-Smith of the New Zealand Nurses Organisation said nurses are in the frontline of helping patients around proper use of antibiotics. “Nurses have an integral part to play. Some nurses are prescribers now and more will come. Education about the importance of taking antibiotics as recommended by a health professional, not sharing them, and reporting adverse effects, is key to managing the use of antibiotics well.”
Wellington GP Dr Cathy Stephenson said it’s crucial to work out whether or not a person really needs an antibiotic.
“It’s partly about explaining to patients why antibiotics won’t help. But it’s also about giving them some practical advice that will help them, or their child, feel better – getting good rest, ensuring adequate fluid intake, and advising on proper pain relief. Often when you explain all this, people are actually very happy to avoid antibiotic use.”
Dr John Wyeth from Pharmac says they are charged with getting the best possible health outcomes for New Zealanders from the public medicines budget – and antimicrobial resistance could undermine that.
“We often forget that things we take for granted, like chemotherapy and surgery, would not be possible without antibiotics.”
Choosing Wisely antibiotic use recommendations
- Do not use antibiotics in asymptomatic bacteriuria.http://choosingwisely.org.nz/professional-resource/asid/#1
- Do not take a swab or use antibiotics for the management of a leg ulcer without clinical infection.http://choosingwisely.org.nz/professional-resource/asid/#2
- Avoid prescribing antibiotics for upper respiratory tract infection.http://choosingwisely.org.nz/professional-resource/asid/#3
- Do not use antimicrobials to treat bacteriuria in older adults where specific urinary tract symptoms are not present.http://choosingwisely.org.nz/professional-resource/anzsgm/#3
- Don’t use oral antibiotics for the treatment of atopic dermatitis unless there is clinical evidence of infection.http://choosingwisely.org.nz/professional-resource/nzds/#4
- Don’t routinely use topical antibiotics on a surgical wound.http://choosingwisely.org.nz/professional-resource/nzds/#5
- Do not routinely prescribe oral antibiotics to children with fever without an identified bacterial infection.http://choosingwisely.org.nz/professional-resource/pchd/#1
- Consider antibiotic de-escalation daily for intensive care patientshttp://choosingwisely.org.nz/professional-resource/anzics/#5
Choosing Wisely also encourages health professionals to share the campaign’s resources for consumers including:
- Antibiotics for sinusitis
- Antibiotics for your skin
- Coughs, colds & sore throats – manage symptoms without antibiotics
- Ear infection – treatments
‘WISE’ questions to help avoid unnecessary prescribing/interventions
- Why? What will this test, treatment or procedure change?
- Is there an alternative? Less invasive, less resource intensive?
- Seek clarification. Clarify why the doctor ordered this test
- Explore/explain. Be the patient’s advocate. Explore concerns, take time to explain why a test, treatment or procedure is/isn’t necessary
Source: From resources developed by the New Zealand Medical Students Association to support the Choosing Wisely campaign: choosingwisely.org.nz/professional-resource/nzmsa/
]]>Tokoroa’s Ka Pai Kai was one response to growing concern over ‘food swamps’ – the over-abundance of unhealthy but ready-to-eat foods in communities, Zaynel Sushil of Waikato District Health Board’s Population Health Unit told the Christchurch conference.
He said very recent research conducted in New Zealand confirmed deprived areas had approximately five times more fastfood outlets and convenience stores than grocery outlets. Exposure to cheap and easy unhealthy food was about three times higher for schools in deprived areas.
“The food environment where we live, work, learn or play influences our food choices. Food swamps and social problems like poverty all follow a similar pattern and some suggest this can lead to a vicious cycle where people are less able to act in their own long-term interests,” he said.
Ka Pai Kai set up a local food network to help the Waikato community work together to build a sustainable local food system. The Ka Pai Kai action plan included food provision, at-risk youth training, café food and waste policy, councils and indigenous food networks.
“It began with a healthy school lunch programme, transformed into a community social enterprise and, since its inception in March 2015, three kohanga, a preschool and nine primary schools have joined.”
This year the Network was recognised by the philanthropy sector as a project for intergenerational change and awarded a significant funding boost, said Sushil.
Healthy school lunches
In another presentation West Coast Community and Public Health Nutrition Health Promoter Jade Winter told the conference about workshops on the West Coast where they provided examples of nutritious and cost-effective lunchboxes.
These included foods such as pasta, carrot sticks, bananas, plain yoghurt, kiwifruit, filled bread cases, boiled eggs, celery sticks, rice crackers, broccoli, hummus and homemade slices.
The cost, at an average of $2.31 per meal, was based on supermarket prices on the West Coast.
“I always explain to parents that providing a healthy lunchbox at a low cost will nearly always require a little time. However, by chopping up extra vegetables at dinner time, or making extra, you are potentially saving time and power!”
Ms Winter said it soon became obvious that parents and caregivers needed a robust, budget-friendly, easy to understand resource so Community and Public Health produced Nourishing Futures with Better Kai. The booklet combines nutrition information and guidelines with practical information such as handy ingredients for the pantry, building a healthy lunchbox, sandwich-filling ideas, healthy party food, dealing with picky eating, oral health and recipes for using leftovers.
Ms Winter said the booklet has had significant input from parents, caregivers, teachers, dietitians, nutritionists and public health professionals to ensure it is as useful as possible.
“Toddlers and young children need appropriate nutrition for growth and development. Eating habits are formed from a very young age and it is important to cultivate these as early as possible. Introducing nourishing foods encourages children to learn about and enjoy different tastes and textures. We hope the resource will help parents and caregivers with that.”
Nourishing Futures with Better Kai is available free on the Community and Public Health website at www.cph.co.nz/wp-content/uploads/nourishingfuturesbetterkai.pdf.
]]>The conference follows a week of ongoing media headlines over concerns about district health board deficits, understaffing and delayed surgery, alongside speculation on which way Winston Peters will swing when coalition talks get underway.
During that week the New Zealand Medical Association also released its Health as an investment position statement that calls for a public debate regarding the level of health funding needed to fulfill the original aims of universal access to comprehensive public health care.
“Nearly 80 years ago New Zealand led the world when we established a public health care system that made health a universal and fundamental right – it’s time our political leaders invest in that promise,” said NZMA chair Dr Kate Baddock.
She said health spending must not be seen as a drain on the economy but as a boost to the economy that improves the lives of New Zealanders. Also required was a commitment to address the social determinants of health such as education, housing and poverty.
Last week NZNO associate professional services manager Hilary Graham-Smith endorsed that by calling for the new government to “get people out of living in cars and damp garages and ensure tamariki are physically and sexually safe”.
“This is not a 100-day aim, this is now, immediately,” Graham-Smith said.
Lindbergh said the PHA endorsed the NZME statement. “As long as government fails to address the underlying causes of illness – poverty, inadequate housing, uncertain work, and educational failure, the health system only will continue to require greater investment,” he said.
He added that cost saving – as the population grew, aged and became more diverse – simply resulted on greater pressure on health services which were now “way beyond reducing costs through so-called ‘efficiences'”.
The senior doctors union, the Association of Salaried Medical Specialists (ASMS), also welcomed the NZMA statement, saying the next government should ensure that spending on our public health service should be seen as an economic and social investment.
“This statement draws attention to international research that indicates other countries are achieving a return on investment of nearly $5 for every $1 of government spending on health,” said Ian Powell, executive director of ASMS.
]]>
Only 20 cases of mumps were reported across the whole of the country last year and Auckland alone has at least 300 cases to date. The disease can be mild for young children but adults who get mumps can experience severe disease.
“Unfortunately we are bearing the brunt of a mumps outbreak in Auckland,” said Dr Josephine Herman, Auckland Regional Public Health’s medical officer of health. The outbreak had now spread to the Waikato and mumps cases were also being reported in smaller numbers across the country.
She said it was looking to the primary health sector and nurses in particular – who are the backbone of primary care – to help promote the MMR (measles, mumps and rubella) vaccine amongst the younger, adolescent population.
Public Health are particularly concerned about a “lost generation” now in their 20s who either did not receive the MMR vaccine in the first place or may have missed out on their second MMR dose when the timing of the second dose was shifted in 2001 from being done at age 11 to age four. They are also at risk of measles and rubella.
Henman said the difficulty was that this age group was generally healthy and independent so didn’t often visit health services. Also the national immunisation register was only 12 years old so it was difficult to identify those who had or hadn’t been vaccinated.
Practice nurses had an important role as families were being urged to check with their family’s general practice to see whether family members had been fully immunised – and also to check their child’s blue Well Child (Plunket) book.
The Immunisation Advisory Centre (IMAC) says the last major mumps epidemic in New Zealand was in 1994 which lead to 188 hospitalistions. Mumps is a viral illness spread by coughing, sneezing and direct contact with infected saliva.
The incubation period (time from infection to onset of symptoms) is on average 16-18 days, and can range from 2-4 weeks. A person with mumps may be infectious from seven days before the salivary glands swell until nine days after.
Henman said for the majority of people who catch mumps it is a mild illness with some painful swelling in the jaw. Some don’t get any swelling with 30 per cent of mumps cases being asymptomatic (though still contagious). But in some cases – with adolescents and adults at higher risk of severe disease from mumps – there can be serious consequences including meningitis, hearing loss and in the case of young and older men it is orchitis (painful swelling and inflammation of the testicles) which in rare circumstances lead to infertility. Henman said women can also have pain through swelling of the ovaries.
According to national immunisation data, the coverage rates in young children up to the age of 12 years are around 80 percent. Today’s mid twenty year olds have even lower rates, with a national coverage survey reporting that only 60 percent of Pakeha children were fully immunised in 1991, with lower rates for Maori (42 percent) and Pacific children (45 percent).
ARPHS has been notified of 300 cases from January 1 to 4 September 2017, with this total greater than all the cases of mumps in the last 16 years. But Henman says there are probably a significant number of cases that have been brought to the services’ attention.
“Mumps is now at large in the community and the only way we can stop this spreading further is to achieve high levels of MMR vaccination in the population,” said Herman.
]]>The Auckland Regional Public Health Service had been notified of 300 cases of mumps from January 1 to September 4 this year.
“Mumps is now at large in the community and the only way we can stop this spreading further is to achieve high levels of MMR vaccination in the population,” Medical Officer of Health Dr Josephine Herman said.
She said the large number of mumps cases meant a large number of people were also at risk of contracting measles and rubella.
“The implications for young adults are deeply concerning, given the risk of non-immune pregnant women catching rubella. This can result in miscarriage or still birth and babies developing severe birth defects,” Herman said.
Mumps also posed a risk of miscarriage for women who were in their first three months of pregnancy, and in rare cases could cause male sterility.
She said there was a “lost generation” where many young people between 10 and 29 had not been vaccinated.
That was partly due to the now discredited MMR controversy from 1998 onwards and a pool of adults who may have missed out on receiving the second dose of the MMR vaccine when they were children when the timing of this dose was moved from 11 years to 4 years in 2001.
Herman said measles was an additional threat to communities with low vaccination coverage.
“It is likely we’ll see further measles outbreaks in schools similar to those in 2011, 2014 and 2016. The measles virus is highly contagious and can lead to serious medical complications as well,” Herman said.
Parents who were unsure about their family’s MMR vaccinations were being urged to check with their practice nurse or look up their children’s blue Well Child book.
According to national immunisation data, the coverage rates in young children up to the age of 12 years were about 80 per cent.
Today’s mid 20-year-olds had even lower rates, with a national coverage survey reporting that only 60 per cent of Pakeha children were fully immunised in 1991, with lower rates for Maori (42 per cent) and Pacific children (45 per cent).
]]>
The film was the brainchild of Sharon Ayto, a public health nurse and the Southern District Health Board’s Child Youth Mortality Coordinator, who won $10,000 in the 2015 Southern Innovation Challenge towards the educational video to teach early childhood teachers and workers how to model safe sleep practices to preschoolers.
Ayto said the inspiration behind the idea was two preschoolers playing with a doll during a wahakura workshop at Awarua Whānau Services in Invercargill. The girls put their ‘baby’ in the pram and covered the doll completely with the available blankets. She realised doll-play was an opportunity to guide ‘tomorrow’s parents’ in safe sleep practices.
Every year in New Zealand about 50 babies die from Sudden Unexpected Death in Infancy (SUDI). SUDI can occur when infants are sleeping in an unsafe sleep environment and many SUDI incidents can be prevented by ensuring every sleep is a safe sleep.
“By introducing safe sleep messages to preschoolers in doll-play, we are creating an ongoing generation of individuals who have safe sleep practices as their norm,” said Ayto. The simple message that teachers are taught to give to preschoolers is Face Up, Face Clear, Safe Place.
Jenny Humphries, Southern DHB’s midwifery director, said it was a wonderful initiative as it was such a simple and innovative idea that could be shared with early childhood teachers and support staff across New Zealand and even wider afield.
Featuring in the film are children from the Southern Institute of Technology (SIT) Early Learning Centre, early childhood teacher Emily Wilson, Change for Our Children founding director Stephanie Cowan, and paediatrician Dr Viliame Sotutu.
The 13-minute video is now available on YouTube.
]]>
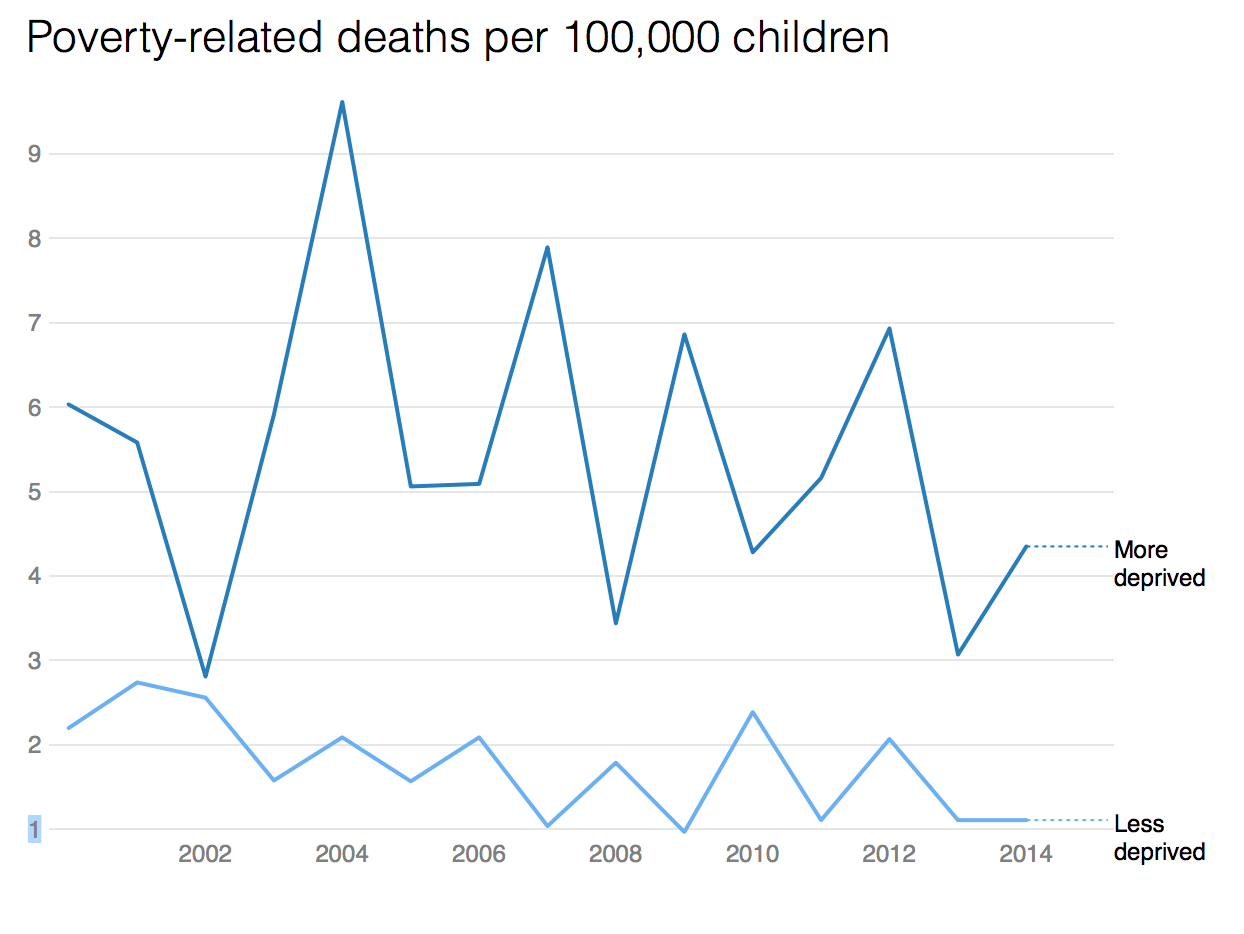
An average 20 children die and 30,000 are hospitalised every year from preventable, housing-related diseases like asthma, pneumonia and bronchiolitis, health statistics show.
(For related full New Zealand Herald investigation article including frustrations with funding of nurse-led healthy housing initiatives click here)
Poor areas suffer the most – suburbs like Auckland’s Pt England and parts of Glen Eden – because of high deprivation and low incomes, lots of rental housing and fewer Europeans.
The illnesses peak in winter. They kill more children than either car crashes or drownings, which claim an average 10 lives a year each.
Health data shows the hospitalisation numbers are climbing. Respiratory conditions in particular – like bronchiolitis and asthma – are causing more hospitalisations each year, with the most severe, such as a “third world” disease named bronchiectasis, irreparably damaging babies’ lungs.
“We have waves of kids coming in the minute it gets cold,” says paediatrician Cass Byrnes.
“We try to delay discharges but the wards are packed. The problem is, the kids just can’t get symptom-free – they go home with antibiotics to the same environment that causes the problem.”
Doctors are calling for an urgent change in housing, saying the combination of child poverty and “shocking” housing conditions have been normalised.
“Inequities in health outcomes will persist unless such stark social inequities are urgently addressed,” the Royal Australasian College of Physicians said.
Interventions by the government have not met demand, doctors said.
Otago University’s Dr Nevil Pierse, deputy director of the housing research unit He Kainga Oranga, said criteria for the Healthy Housing Initiative – initially aimed only at families at risk of rheumatic fever – were too strict and many families were missing out.
The initiative missed children suffering from common conditions like asthma and skin infections, and was also limited to the poorest families.
Nurses were funded to assess houses, but then the money dried up, and families relied on charity or their landlord to provide the required provisions such as curtains, bedding, or insulation.
Data shows that of the 5500 families referred so far, 4020 were assessed.
An average 60 per cent of those who needed them received curtains or floor coverings, but only 34 per cent of recommended insulation was installed. Just 25 per cent of families nominated for new houses were able to move, because of the housing crisis.
“Basically, they’re doing the right thing but they’re doing it too cheaply. There’s not enough kids, not enough criteria, not enough help,” Pierse said.
“It’s just ridiculous – if there was a new pill they would spend the money. If there was a pill as effective as good quality housing the health sector would spend the money so why don’t they spend it on this?”
Those working in the field said one of the biggest barriers to progressing interventions like insulation were landlords – who had to pay half the cost.
Ministry of Health spokesperson Dr Stewart Jessamine said the environment in which the interventions worked was “complex and challenging” as staff had to liaise with multiple agencies.
He said sometimes it was difficult to contact the families as well as landlords. Landlords were able to decline interventions, he said.
Despite the difficulties, the ministry considered the project a success and many more thousands of families were expected to benefit in the coming years, particularly with “vulnerable” families now included in risk criteria.
Health minister Jonathan Coleman said the housing interventions would be continued as part of the government’s new target of reducing avoidable child hospitalisations by 25 per cent in five years.
It will also “work in partnership” with other agencies to reduce housing-related health conditions. He did not describe what that would entail.
‘Bronchiectasis: It’s completely terrifying’
When Niki Te Puni said the name of her daughter’s disease over the phone, her mum went silent at the other end.
“That’s when I knew it was bad,” Te Puni says. “Mum’s a paediatric nurse and she knew exactly what it was. I couldn’t even pronounce it.”
Te Puni’s daughter Kierra, then just 2 years old, had been diagnosed with bronchiectasis, an irreversible, life-threatening lung disease caused by repeated chest infections.
Kierra, now 5, was among 99 children to be diagnosed with the condition that year. Rates have kept climbing since, and now 300 New Zealand kids have a disease that should be confined to geriatrics.
“It’s a third-world disease, the kind of thing that if you were going to see it, the patients would be in their 80s,” says Byrnes, from Starship children’s hospital.
“Internationally people are astonished at the numbers we have here. It’s completely terrifying.”
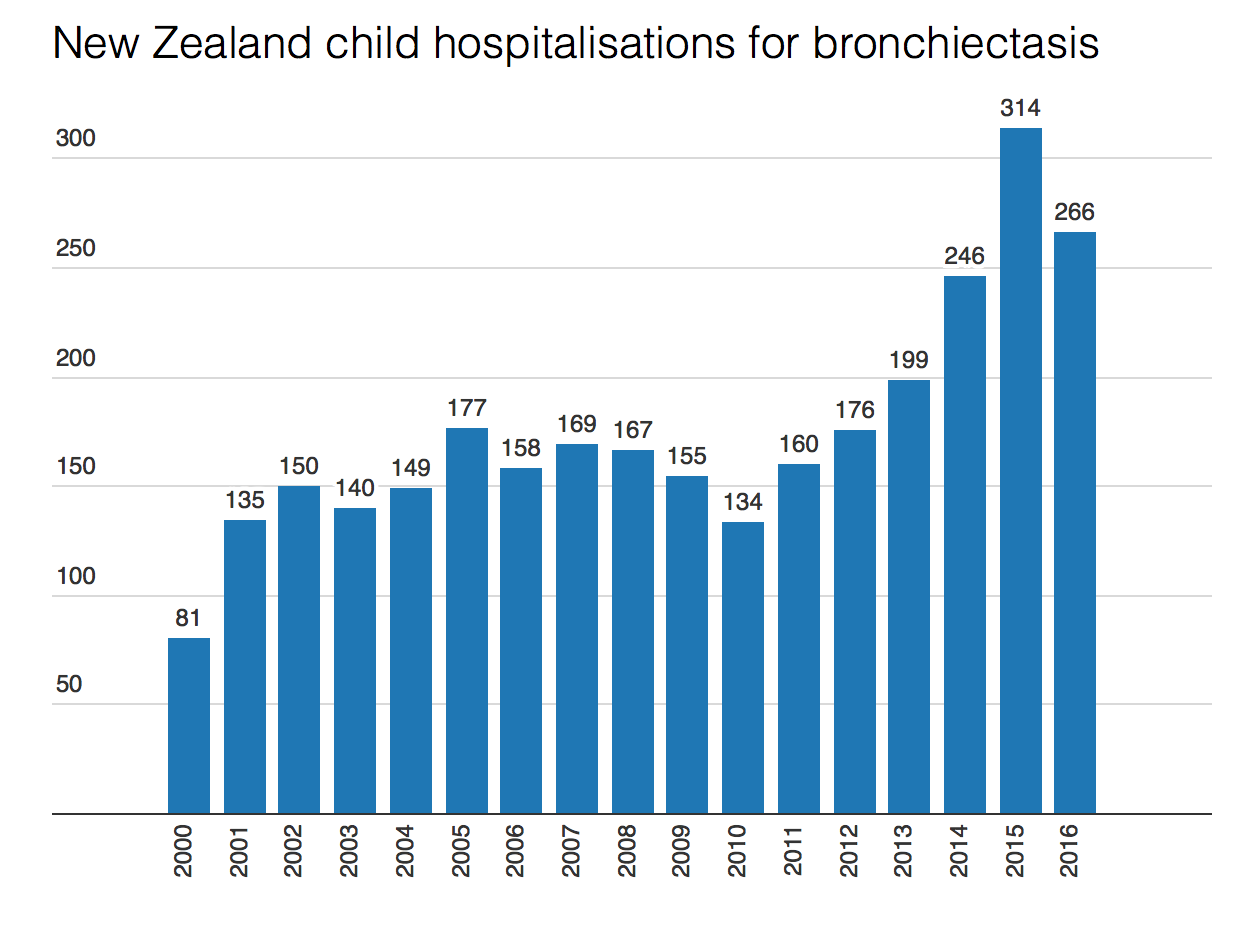
Bronchiectasis is caused by scarring in the lungs, which allows mucus to build up and leads to ongoing infections. It’s linked to cold housing, and other unhealthy conditions like dampness, or inside smoking. It can be fatal.
When Kierra was diagnosed, a young girl the family knew in Whangarei had just died from it.
“It was heart-wrenching,” Te Puni says. “And it’s exhausting. We are constantly at the doctors, constantly making Kierra wear a jacket, a beanie, shoes. Even though she loves shorts.”
They also replaced a gas heater with a heat pump, to warm their high-ceilinged older home.
Te Puni says she wants to raise awareness about the disease, to let others know it’s not normal for kids to be coughing all the time, or to have a snotty nose.
The family are determined to give Kierra as normal a life as possible. Sometimes it’s not easy: she gets bored of her breathing exercises and just wants to be like the other kids. It can be a struggle not knowing if her condition will worsen in time.
“I have no idea what’s ahead for us,” Te Puni says. ” What’s in our future next week or next year. Sometimes we feel like the only ones going through it.”
]]>Doors will open at 5pm on Tuesday August 29 at Nga Taonga Sound and Vision, 84 Taranaki St, Wellington, with MC Linda Clark. The debate will also stream live on Facebook.
]]>