Rosie Winters, an Older Adult Nurse Practitioner, said staff got in their pyjamas to launch their Let’s Get Moving campaign. “We wanted to start a conversation about the impact even a few days’ bed rest can have on reducing muscle strength and increasing the risk of complications for patients, particularly for older patients in hospital,” said Winters.
Key themes of the week included a focus on getting patients dressed in their normal clothes again as soon as possible and staying active. Patient feedback was very positive and the experience of wearing pyjamas to work proved thought-provoking for staff.
“One of our staff said how unmotivated she felt because she was wearing her pyjamas,” said Winters. “It brings home the psychology of clothes. We’ve used this as an opportunity to talk to patients about being conscious of their activity levels each day.
“With patients, once they come in and change into gowns they tend to retract into a passive role. For the older person even a few days’ bed rest can cause a rapid decline in muscle strength and lead to an increased stay in hospital and complications.”
The Bay of Plenty Let’s Get Moving campaigns is based on the #endPJparalysis movement co-founded by Christchurch-based nurse and consultant Brian Dolan.
The #endPJparalysis movement was started early this year by Dolan, who spends part of the year based in the UK, and his Irish business partner as a twitter hashtag linking twitter conversations on the topic of getting older patients up and dressed.
The West Coast DHB was the first DHB to get behind the movement, with medical ward clinical nurse manager Rose Kennedy saying it provided a framework for medical wards like her own to support a restorative model of care and hadn’t added to the nursing workload, just reshaped it.
]]>Nurses are the largest health professional group in a sector that takes a lion’s share of government funding.
Nurses deliver health care to young and old, rich and poor and the healthy to the dying, which gives them a unique insight into the state of our health system. Nurses have political views as diverse as any other section of the public, but share a common interest in wanting to do the best for their patients and clients.
This election the New Zealand Nurses Organisation’s election manifesto has also been supported and endorsed by the College of Nurses Aotearoa New Zealand.
The Nursing Matters manifesto sets out seven priorities for nursing and public health. Nursing Review gives a brief summary of how the released election policies to date of the five main political parties stack up against those seven priorities, plus mental health.
(See links to full health policies of the eight political parties in the running at bottom of article. The parties in that list and below are in alphabetical order.)
Nursing Matters Priorities
- A SUSTAINABLE, FULLY UTILISED NURSING WORKFORCE (N.B. We have included specific references to nursing in parties’ online policies here)
GREENS: Have a school nurse in every low decile school. Visits to nurses or doctors free for under-18s. Improve palliative care training for medical, nursing and allied health staff in hospitals, hospices and aged care facilities.
LABOUR: Extend nurse-led school-based health service. Fund an additional 100 Plunket and Tamariki Ora nurses.
NATIONAL: Introduce registered nurse prescribing. Nursing and doctor numbers employed in DHBs have increased by 6,900 in past nine years.
- INVESTMENT IN PUBLIC HEALTH
GREENS: Match increasing need for health services with increased funding.
LABOUR: An additional $8 billion investment in health over four years to meet inflation and demographic pressures and address current funding shortfalls.
MĀORI: Establish a new Māori and Pacific social investment fund managed by the Māori Pasifika Health Commissioning Unit.
NATIONAL: Health top funding priority, with Vote Health budget increased by $888 million for 2017-2018 to $16.8 billion. Increase number of elective surgeries to 200,000 a year by 2021. Social investment package.
NEW ZEALAND FIRST: Establish public health compact stipulating guaranteed minimum services. Adequately resource elective surgery and establish guaranteed maximum waiting times for surgical/specialist treatment.
- A PRIMARY HEALTH CARE APPROACH TO IMPROVING POPULATION HEALTH
GREENS: Review funding formula for primary care, specifically looking at high needs populations. Visits to nurses or doctors free for under-18s.
LABOUR: Cut GP fees by $10 a visit with $8 GP visits for community service cardholders. Review funding of primary care system. Review current funding model for residential aged care and update national baseline aged care standards.
MĀORI: Free annual and medical and dental visit for over-55s. Free GP visits and dental care for under-18s. Increase kaupapa Māori services. Increase mobile health clinics in rural communities. Explore the rollout of IMOKO nationwide. More Whānau Ora navigators.
NATIONAL: Cap the cost of GP visits to $18 for people with community services cards (estimated up to 600,000 extra New Zealanders could be eligible). Support family health hubs. Introduced Health Families NZ policy and combined phone helplines.
NEW ZEALAND FIRST: Review funding of primary health organisations. Introduce three annual GP visits for over-65s (SuperGold card). Fully fund palliative care services.
- ORANGA TAMARIKI – THE HEALTH AND WELLBEING OF CHILDREN AND YOUNG PERSONS
GREENS: Visits to nurses or doctors free for under-18s. Have a school nurse in every low decile school (see also mental health). Every baby gets baby pod at birth. Ensure only healthy food and drink sold at schools.
LABOUR: Extend nurse-led school-based health services to all public secondary schools. Extend paid parental leave from 18 weeks to 26 weeks. Support healthy eating and nutrition for children. Set child obesity reduction target and rollout Waikato’s Project Energize programme. Review Youth One Stop Shop funding (see also social and health equity priority).
MĀORI: Free GP visits and dental care for under-18s. Introduce mental health counsellors in all high schools. Subsidise power bills for those with rheumatic fever.
NATIONAL: New target of keeping children out of hospital for preventable conditions. Free GP visits and prescriptions for under-13s. Parents and newborns package including extending paid parental leave to 22 weeks. Ongoing policies include childhood obesity plan, Fruit in Schools and meeting B4 School Check and immunisation targets (see also social and health equity priority).
NEW ZEALAND FIRST: Nationwide health screening of all children under one-year (see also mental health). Support increasing paid maternity leave to 26 weeks and paid paternal leave of two weeks rising to four weeks.
- SAFE CLINICAL ENVIRONMENTS (see also investment in public health priority)
GREENS: Implement solutions to health workforce problems that have been jointly developed by health professionals.
LABOUR: Commit to building new hospital for Dunedin.
MĀORI: Increase in kaupapa Māori service.
NATIONAL: Invest in new hospitals in Christchurch, Greymouth, Dunedin. DHBs employing 6,900 more doctors and nurses than nine years ago. Establish a School of Rural Medicine.
NEW ZEALAND FIRST: Review number of district health boards (DHBs) and establish a ratio of practitioners to administrators.
- FAIR EMPLOYMENT
GREENS: Amend pay equity laws. Require all workplaces to measure and disclose pay gap between genders (see Labour below).
LABOUR: Pledged to scrap Pay Equity legislation currently in parliament. Make mental health workers a priority in pay equity negotiations. Labour and Greens Inquiry into Aged Care report notes pay equity settlement has created issues and funding concerns for sector, including loss of pay relativity for registered nurses.
MĀORI: No specific pay equity policy online. Introduce living wage for all workers.
NATIONAL: Introduced $2 billion pay equity settlement for 55,000 residential aged care and care workers. Legislation for pay equity framework currently before parliament.
NEW ZEALAND FIRST: Provide equality of funding for all family home carers. Review aged care sector funding – particularly rest home funding after pay equity.
- SOCIAL AND HEALTH EQUITY IN AOTEAROA
GREENS: Link benefits to fixed percentage of average wage, introduce universal child benefit (that can be capitalised for first home), tax free zone for first $10,000, look at benefit abatement for beneficiaries working part-time. Increase state housing units, expand social housing, more secure tenancy conditions and increase low-interest housing finance for low-income households.
LABOUR: Lift 100,000 children out of poverty by 2020. Legislate a child poverty reduction target. Implement a families package including Best Start scheme payments for children up to age of three for low and middle-income earners, continue with accommodation supplement increases and boost access to Working for Family payments. Increase minimum wage to $16.50 an hour and promote Living Wage. Stop sale of state houses and build more. Pass Healthy Homes Guarantee Bill to ensure rental properties warm and dry. Build 100,000 more affordable houses over 10 years. Implement rental reforms. Change Public Finance Act so Budget reports on reducing child poverty
MĀORI: Cost of living adjustment to all benefits. Introduce living wage. Housing policy includes developing National Housing Strategy, improve renters rights, enforce compulsory rental home warrant of fitness, provide low interest housing loans and introduce options for ‘rent to buy’.
NATIONAL: Family Incomes package from next year will shift tax thresholds for low income families, lifting Family Tax Credit up to age 18 and increasing accommodation supplement rates next year. PM Bill English says this will lift 50,000 children out of poverty and he pledges to bring another 50,000 children out of poverty by 2020 if re-elected. Increase social housing available from 66,400 to $72,000 over three years. Announced plan to build 34,000 new houses in Auckland in next 10 years. Budget had $20 million over four years for more emergency and transitional housing, expansion of Housing First programme for homeless and extending Warm and Dry upgrades of social housing. Would double HomeStart grants for first homebuyers.
NEW ZEALAND FIRST: Raise minimum wage to $20 an hour over next three years. Greater scrutiny of the benefit system, adjustment benefits and abatement levels. Remove secondary tax. Introduce flexible state support for grandparents raising grandchildren.
- MENTAL HEALTH
GREENS: Free counselling for all New Zealanders under 25 and increase youth mental health funding by $100 million a year. Support an independent inquiry into mental health
LABOUR: Initiate review of mental health and addiction services in first 100 days to identify gaps in services. Two-year pilot of basing primary mental health teams at eight primary health centre sites in high needs areas to offer early intervention and continuing care. Teams led by ‘doctors or other medical professionals’.
MĀORI: Expand Rangatahi Suicide Prevention Strategy. Increase kaupapa Māori mental health and addiction services. Support an independent inquiry into mental health. Reduce tobacco supply and subsidise e-cigarettes. Eliminate synthetic cannabis. Increase respite care beds for P-addicts.
NATIONAL: Increased funding announced in Budget including $100 million over four years for 17 social investment initiatives and pilots. Mental health funding services increased from $1.1 billion to $1.4 billion. Moving to emphasis on mental wellness, resilience and new ways of accessing services.
NEW ZEALAND FIRST: Re-establish Mental Health Commission. Commit to a suicide reduction target. Support an independent inquiry into mental health. Increase mental health service options and beds especially around child and youth mental health services.
HEALTH POLICY LINKS
ACT: http://act.org.nz/health/
Greens: https://www.greens.org.nz/page/health-policy
Labour: http://www.labour.org.nz/health
Māori: http://www.maoriparty.org/health_policy_2017
National: https://www.national.org.nz/health
New Zealand First: http://www.nzfirst.org.nz/health
The Opportunities Party: http://www.top.org.nz/top15
United Future http://unitedfuture.org.nz/our-policies/
]]>
A great deal of research in recent years has focused on the benefits of mobilising all patients as soon as possible after surgery. Mobilising after hip or knee replacement surgery (lower limb arthroplasty or LLA), however, has traditionally been delayed. But advancements in surgical and anaesthetic technique mean it is now not only safe to mobilise these patients earlier, but there is also evidence that there are many benefits in doing so.
Background
Arthrosis – the degeneration of a joint most commonly caused by osteoarthritis – is the leading reason for having joint replacement surgery or arthroplasty. Arthrosis is debilitating, often causing pain and disability and substantially reducing the quality of life of those affected.
The first attempts at joint replacement surgery happened more than 100 years ago, but only became effective in the 1960s (1,2). Hip and knee replacements (LLA) have become more common in the last two decades and, with our ageing population, demand will continue to grow (it is estimated that arthrosis affects 75 per cent of people over 65).
To meet this growing demand, researchers are looking at ways to reduce costs. Traditionally, LLA patients spent extended periods of time recovering in hospital. While length of stay has reduced for all types of surgery in the past 10 years, there is still a huge variability in length of stay globally after LLA, with ranges of 1–21 days (4).
A number of enhanced recovery programmes (ERPs) – also known as enhanced recovery after surgery (ERAS) or ‘fast track’ protocols – have gained popularity in Europe and the US, with beneficial results for both LLA patients and providers (5). Many ERPs are expensive to implement, however, with entire units set up with increased staffing and equipment.
But while researching the barriers and opportunities for LLA patients in my own hospital (as part of a nursing research methods paper), I found one key component of many ERPs that I felt could be hugely beneficial as a stand-alone change: mobilising LLA patients on the day of surgery, not the day after. This became the focus of my master’s degree research. (Mobilising the day after surgery, i.e. day one, was standard when I began the study. See sidebar 1 for a summary of literature review findings on the benefits of early mobilisation of LLA patients.)
Introducing day of surgery mobilisation
Like many idealistic students, I wanted to carry out a randomised controlled trial to compare outcomes between day of surgery and day one mobilisers. However, my literature review revealed so many benefits in mobilising early, that I decided it would be unethical to make some patients stay in bed and not have the opportunity to benefit.
So, with the support of our surgeons and management at my 38-bed private surgical hospital in New Plymouth, I introduced an early mobilisation initiative for LLA patients as a quality improvement project. The initiative included developing a checklist so nurses could be confident that their patients were safe to mobilise (see checklist box). Three months later, after receiving ethics consent, I audited the discharged patient files for my master’s thesis and compared the outcomes of early mobilised LLA patients with the outcomes of patients mobilised on day one.
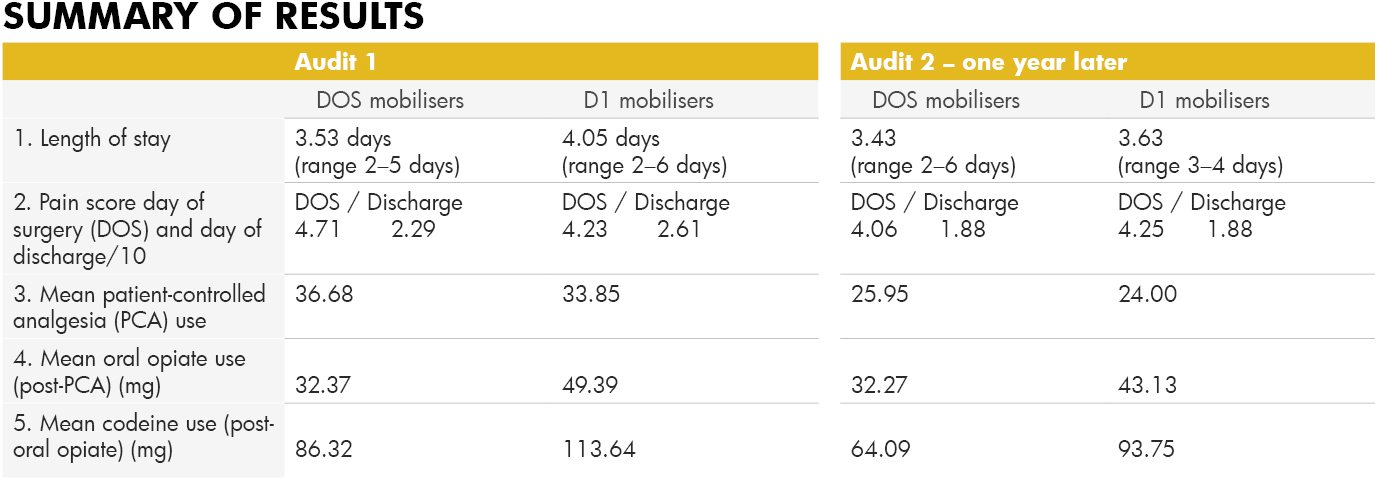
Exactly a year after the first audit, I conducted a follow-up audit. This was partly because uptake of the idea at the beginning was relatively slow, but gained support over the year as nurses and surgeons saw the benefits to patients. I also wanted to ensure that the gains were sustained (see sidebar 2 for audit results).
Conclusion
Many nurses were initially sceptical about mobilising LLA patients on the same day as their surgery. But the initiative soon gathered momentum when nurses saw for themselves their patients gaining independence earlier, with less pain and fewer adverse effects post-surgery.
This change of heart was reflected in the audit results with only 56 per cent of LLA patients being mobilised successfully on the day of surgery in the first audit, compared with 84.6 per cent a year later.
While pain scores on the day of surgery were slightly higher on the day of surgery for early mobilisers, by the day of discharge their scores were lower, and less pain relief was used by early mobilisers during their stay, indicating lower pain levels. The length of stay decreased after the initiative and continued to decrease in the follow-up. Early mobilisation after LLA has now become the norm at our hospital as we continue to see improved outcomes for these patients.
*Author: Diane Alder Is a registered nurse at New Plymouth’s Southern Cross Hospital and completed a Master of Health Sciences degree last year.
Sidebar 1:
The benefits of early mobilisation of LLA patients
-
Less risk of venous-thromboembolism (VTE)
Patients mobilised the day of surgery are 30 times less likely to suffer from VTE complications (6).
-
Less pain
A number of studies show early mobilisers state lower pain scores overall (7,8,9). And the benefit isn’t just short-term; a German study found their early mobilisation group stopped taking analgesia altogether by day 41, while the traditional day one mobilisers continued to take analgesia for a further 30 days (10).
-
Less opiate pain relief required
Lower pain scores means less pain relief. One study showed a 60 per cent reduction in opiate use in the early mobilising group (6). Less opiate medication means a reduction in side effects, such as nausea and vomiting, so a reduced need for anti-emetics.
-
Less syncope
Often cited as a reason not to mobilise on the day of surgery, the risk of syncope is actually less likely to occur (6). Judicial intravenous fluid replacement and good pre-mobilising assessment is, of course, important.
-
Fewer blood transfusions
Fear of increased blood loss is also cited as a reason not to mobilise but early mobilisers actually have less need for blood transfusions – 9.8 per cent compared with 23 per cent (6,11).
-
Less joint stiffness
Joint stiffness can be associated with chronic pain following LLA. A Danish researcher found that early and intensive mobilisation helped to avoid the development of specific knee arthroplasty complications such as prolonged stiffness and delays in recovery of strength (12, 13).
-
Less mortality
Several large studies show that mortality reduces with ERPs that include early mobilisation (11,14,15).
-
Less time in hospital
Fifteen recent studies showed a reduced length of stay with ERPs; five of the studies isolated early mobilisation and studied its effect on length of stay. Results varied but 100 per cent had reduced length of stay for early mobilisers.
-
Increased quality of life/satisfaction
Most patients would prefer to be home, back to work or back to the golf course as soon as possible. A Danish study showed early mobilisers had increased quality of life/satisfaction (16).
-
Fewer infections
Many studies show shorter lengths of stay mean fewer infections, (8, 10, 17, 18). If a patient is able to mobilise to the toilet within hours of having LLA surgery, there is no need for an indwelling urinary catheter, removing the risk of catheter-induced UTIs. The less time a patient is in bed, the less chance of orthostatic pneumonia. And less time in hospital means a reduced likelihood of a hospital-acquired infection.
-
Fewer re-admissions
Early opponents to fast-track protocols argued that, if discharged too early, patients would just return as re-admissions. In fact, patients who mobilise earlier are far less likely to be re-admitted (4,19).
-
Economic benefits
There are huge savings to be made with reduced length of stay. Several studies have researched the economic benefits, citing savings of US$454,000 per annum in just one hospital in the US (20), €3.5 million in total per annum in Denmark (15), and £141 million in total per annum in the UK (11).
Side bar 2:
Early mobilisation New Zealand clinical audit
Audit 1: December 2015, following the introduction of an early mobilisation initiative for LLA patients in September 2015.
Subjects: n=52 (pre-initiative) + n=52 (post-initiative) = 104 patients, split into two groups; those that mobilised day of surgery (DOS) n=38; and those that mobilised day one (D1) n=66. Age range of patients was 51–92 years.
Audit 2: Follow-up audit. December 2016, one year later.
Subjects: n= 52, divided into DOS mobilisers n=44 and D1 mobilisers n=8.
Safety criteria checklist for early mobilisation
1. Patient is haemodynamically stable
● Blood pressure is stable, with systolic ≥ 100
● Heart rate is stable ≤ 100bpm
● Bleeding is minimal-moderate, if drain used then ≤ 50ml/hour
● Patient is not light-headed or short of breath at rest
2. Patient is neurovascularly stable
● Patient can actively plantar and dorsi flex ankles of both feet
● Patient can actively contract both quadriceps (doesn’t necessarily have to lift leg actively)
● Sensation can be reduced in operated leg, but not absent
3. Patient consent
Patient is alert and oriented and able to consent to mobilising
● Pain is controlled to level considered acceptable to patient at rest
REFERENCE LIST
- Wroblewski, B. M., Siney, P. D., & Fleming, P. A. (2006). The charnley hip replacement: 43 years of clinical success. Acta Chirurgiae Orthopaedicae et Traumatologiae Cechoslovaca, 73(1), 6-9.
- Mont, M., Jacobs, J., Lieberman, J., Parvizi, J., Lachiewicz, P., Johanson, N., & Watters, W. (2012). Preventing venous thromboembolic disease in patients undergoing elective hip and knee arthroplasty. (2011). The Journal of the American Academy of Orthopaedic Surgeons, 19(12), 768.
- Lilikakis, A. K., Gillespie, B., & Villar, R. N. (2008). The benefit of modified rehabilitation and minimally invasive techniques in total hip replacement. Annals of the Royal College of Surgeons of England, 90(5), 406-411. doi:10.1308/003588408X285900
- Stambough, J. B., Nunley, R. M., Curry, M. C., Steger-May, K., & Clohisy, J. C. (2015). Rapid recovery protocols for primary total hip arthroplasty can safely reduce length of stay without increasing readmissions. The Journal of Arthroplasty, 30(4), 521-526. doi:10.1016/j.arth.2015.01.023
- Bandholm, T., & Kehlet, H. (2012). Physiotherapy exercise after fast- track total hip and knee arthroplasty: Time for reconsideration? Archives of Physical Medicine and Rehabilitation, 93(7), 1292-1294. doi:10.1016/j.apmr.2012.02.014
- Pearse, E. O., Caldwell, B. F., Lockwood, R. J., & Hollard, J. (2007). Early mobilisation after conventional knee replacement may reduce the risk of post-operative venous thromboembolism. Journal of Bone and Joint Surgery-British Volume, 89B(3), 316-322. doi:10.1302/0301-620X.89B3.18196
- Lunn, T. H., Kristensen, B. B., Gaarn-Larsen, L., & Kehlet, H. (2012). Possible effects of mobilisation on acute post-operative pain and nociceptive function after total knee arthroplasty. Acta Anaesthesiologica Scandinavica, 56(10), 1234-1240. doi:10.1111/j.1399-6576.2012.02744.x
- Labraca, N. S., Castro-Sanchez, A., Mataran-Penarrocha, G., Arroyo-Morales, M., Sanchez-Joya, M., & Moreno-Lorenzo, C. (2011). Benefits of starting rehabilitation within 24 hours of primary total knee arthroplasty: Randomized clinical trial. Clinical Rehabilitation, 25(6), 557-566. doi:10.1177/0269215510393759
- Raphael, M., Jaeger, M., & van Vlymen, J. (2011). Easily adoptable total joint arthroplasty programme allows discharge home in two days. Canadian Journal of Anesthesia-Journal Canadien d Anesthesie, 58(10), 902-910. doi:10.1007/s12630-011-9565-8
- den Hertog, A., Gliesche, K., Timm, J., Muhlbauer, B., & Zebowski, S. (2012). Pathway-controlled fast-track rehabilitation after total knee arthroplasty: A randomized prospective clinical study evaluating the recovery pattern, drug consumption, and length of stay. Archives of Orthopaedic and Trauma Surgery, 32(8), 1153-1163. doi:10.1007/s00402-012-1528-1
- Malviya, A., Martin, K., Harper, I., Muller, S. D., Emmerson, K. P., Partington, P. F., & Reed, M. R. (2011). Enhanced recovery programme for hip and knee replacement reduces death rate: A study of 4,500 consecutive primary hip and knee replacements. Acta Orthopaedica, 82(5), 577-581. doi:10.3109/17453674.2011.618911
- Holm, B., Kristensen, M. T., Myhrmann, L., Husted, H., Andersen, L. O., Kristensen, B., & Kehlet, H. (2010). The role of pain for early rehabilitation in fast track total knee arthroplasty. Disability and Rehabilitation, 32(4), 300-306. doi:10.3109/09638280903095965
- Husted, H., Jørgensen, C. C., Gromov, K., & Troelsen, A. (2015). Low manipulation prevalence following fast-track total knee arthroplasty: A multicenter cohort study involving 3,145 consecutive unselected patients. Acta Orthopaedica, 86(1), 86-91.
- Savaridas, T., Serrano-Pedraza, I., Khan, S. K., Martin, K., Malviya, A., & Reed, M. R. (2013). Reduced medium-term mortality following primary total hip and knee arthroplasty with an enhanced recovery programme: A study of 4,500 consecutive procedures. Acta Orthopaedica, 84(1), 40-43. doi:10.3109/17453674.2013.771298
- Khan, S. K., Malviya, A., Muller, S. D., Carluke, I., Partington, P. F., Emmerson, K. P., & Reed, M. R. (2014). Reduced short-term complications and mortality following enhanced recovery primary hip and knee arthroplasty: Results from 6,000 consecutive procedures. Acta Orthopaedica, 85(1), 26-31. doi:10.3109/17453674.2013.874925
- Larsen, K., Sorensen, O. G., Hansen, T. B., Thomsen, P. B., & Søballe, K. (2008). Accelerated perioperative care and rehabilitation intervention for hip and knee replacement is effective: A randomized clinical trial involving 87 patients with 3 months of follow-up. (2008). Acta Orthopaedica, 79(2), 149-159. doi:10.1080/17453670710014923
- Tayrose, G., Newman, D., Slover, J., Jaffe, F., Hunter, T., & Bosco, J. (2013). Rapid mobilization decreases length-of-stay in joint replacement patients. Bulletin of the NYU Hospital for Joint Diseases, 71(3), 222-226.
- Wellman, S. S., Murphy, A. C., Gulcynski, D., & Murphy, S. B. (2011). Implementation of an accelerated mobilization protocol following primary total hip arthroplasty: Impact on length of stay and disposition. Current Reviews in Musculoskeletal Medicine, 4(3), 84-90. doi:10.1007/s12178-011-9091-x
- Robbins, C. E., Casey D., Bono, J. V., Murphy, S. B., Talmo, C. T., & Ward, D. M. (2014). A multidisciplinary total hip arthroplasty protocol with accelerated postoperative rehabilitation: does the patient benefit? The American Journal of Orthopedics, 43(4), 178-181.
- Chen, A. F., Stewart, M. K., Heyl, A. E., & Klatt, B. A. (2012). Effect of immediate postoperative physical therapy on length of stay for total joint arthroplasty patients. Journal of Arthroplasty, 27(6), 851-856. doi:10.1016/j.arth.2012.01.011
The findings are the latest analysis from the RN4CAST study that connected nursing levels, the outcomes of more than 400,000 patients and survey data from 25,000 nurses working across 300 hospitals in nine European countries (including England, the Netherlands and Ireland). The latest research was lead by Dr Jane Ball of the University of Southampton and fellow authors included co-director of the RN4CAST study, Professor Linda Aiken of the University of Pennsylvania.
Ball said for years it was known there was a relationship between nurse staffing levels and hospital variation in mortality rates, but there had not been a good explanation as to how or why. However, links had now been found between lower RN staffing levels, missed patient cares and increased risks of patient death. Each 10 per cent increase in cares left undone was associated with a 16 per cent increase in the likelihood of a patient dying.
The study analysed nurses’ responses to the survey question: “On your most recent shift, which of the following activities were necessary but left undone because you lacked the time to complete them?” and presented nurses with a list of 13 activities (see list below).
The nurses surveyed were also asked how many staff were providing direct care on their last shift and how many patients were on the ward at the time.
Previous analysis of the survey showed that lower nurse staffing levels are associated with higher mortality, but Ball said the further analysis gave the “clearest indication yet that RN staffing levels were not just associated with patient mortality, but that the relationship may be causal”.
“If there are not enough registered nurses on hospital wards, necessary care is left undone and people’s lives are put at risk,” added Dr Ball.
Co-author Luk Bruyneel from KU Leuven in Belgium said the findings had implications for healthcare managers and policymakers. “Monitoring missed care may offer a more responsive and sensitive early-warning system for hospitals to detect problems before patients die,” he said. “More work needs to be done worldwide to ensure we utilise this data for the benefit of patients.”
The analysis also looked at nurses’ qualifications and confirmed that hospitals with higher numbers of registered nurses trained at degree level had a lower risk of patient mortality.
Professor Peter Griffiths, Chair of Health Services Research at the University of Southampton, said the study reinforced the importance of RNs who were trained to degree level. “It is more evidence that shows that you cannot substitute fully qualified RNs with less qualified staff without taking a risk with patient safety,” said Griffiths. “It is the number of RNs on duty that is key to ensuring complete care and minimising the risk of patients dying.”
Article reference:
Jane Ball, Luk Bruynell, Linda H. Aiken et al (2017). Post-operative mortality, missed care and nurse staffing in nine countries: A cross-sectional study. International Journal of Nursing Studies (published online open access)
The patient cares asked about in the RN4CAST nursing survey were:
- adequate patient surveillance
- skin care
- oral hygiene
- pain management
- treatments and procedures
- administering medication on time
- frequently changing the patient’s position
- comforting/talking with patients
- educating patients and family
- preparing patients and families for discharge
- developing or updating nursing care plans/care pathways
- documenting nursing care
- planning care.
]]>
The NZNO College of Emergency Nurses NZ (CENNZ) was responding to a press release yesterday from Health Minister Jonathan Coleman stating that the nationwide health targets – including the ‘shorter stays in ED‘ target – were making a real difference to the quality of care and saving lives. The latest target data shows that 93 per cent of patients were admitted, discharged or transferred from emergency departments (EDs) around the country within six hours. Coleman said that recent New Zealand research indicated that the ‘shorter stay’ target was saving lives, with an estimated “700 fewer deaths than predicted in 2012 if pre-target trends had continued”.
The College said their outrage at the minister claiming the target as a success was because nurses knew that meeting the ED target in “an underfunded health system” could “cost lives and careers”.
Hilary Graham-Smith, NZNO’s associate professional services manager, also pointed to the recent Health & Disability Commissioner’s report into the death of a Northland man who was moved out of ED specifically to meet the national target when he had a heart condition needing further assessment. She said “trumpeting the targets” just days after that news was “inappropriate”.
Chairperson of CENNZ, Rick Forster said members told him that ED occupancy rates were often well over 100 per cent and ED staff faced additional difficulties trying to admit patients to the wards because hospital beds were full.
“When ED’s full we can’t close the doors, so more patients are ending up in corridors,” said Forster. “There comes a tipping point where care is rationed and risk of harm increases.”
Graham-Smith said the ED targets needed to be re-examined and nurses consulted. She said the combined effect of a high-needs and ageing population, patients with complex needs and several particularly bad winters had resulted in ED staff feeling they were compromising the quality of care and patient safety. EDs were also facing a staff shortage crisis.
She backed Forster’s comments and said New Zealanders did not deserve to be left waiting for extended periods in ED waiting rooms, in ambulances or on trolleys in corridors.
“Nurses need to be able to provide safe and effective care that is of a high standard, and the time to do that should not be constrained by a national target,” said Graham-Smith. “The stress of care rationing on nurses is unacceptable to the nursing profession and NZNO.”
Coleman acknowledges ED nurses work
Coleman responded on August 24 to the College and NZNO comments saying he acknowledged the work of nurses across the health system “particularly among the pressures which do arise in any busy ED, especially in the middle of winter”.
He said the shorter stays target helped to address “formally unsafe and long ED waiting times which were known to put lives (and potentially careers) at risk”.
The minister said the Emergency specialist Mike Ardagh’s research cited in his initial press release indicated the target had lead to an overall reduction in hospital stays by an average of about seven hours, created capacity for more acute admissions and equated to 700 fewer deaths than expected if pre-target trends continued.
He said the health system wasn’t underfunded with health funding having kept ahead of demographic pressure and inflation over the past eight years. “Health has remained the Government’s number one funding priority,” said Coleman. “Budget 2017 delivers on that by investing an extra $3.9 billion in health over four years for new initiatives and to meet cost pressures and population growth.” He said the health budget would reach an record $16.8 billion in 2017/18.
Article updated 10am August 24
]]>Clinical director Dr David Richards says the department normally has about 250 admissions a day at this time of year, but in the past three weeks it’s been more like 300.
He says the hospital has been at capacity, so on average they’re having to treat 10 or 12 patients in the ED corridors, which he says is “unacceptable”.
“It’s unpleasant for the patients and family members, it means staff have to navigate the trolleys, and it provides very little privacy,” he said.
]]>
In his report, Hill acknowledged that the hospital’s emergency department (ED) was exceptionally busy the day that ‘Mr B’ presented for the second time in just over a week. He also acknowledged the Ministry of Health target was for patients to be transferred from ED within six hours, but he said that it was unacceptable for Mr B to have been transferred to a surgical ward “in order to meet a target” when it was clinically inappropriate.
His report found that ED ‘busyness’ had resulted in delays in triage, important aspects of Mr B’s management plan (including insertion of a catheter and commencement of a fluid balance chart) not being started while he was in ED, and also extended delays in a requested medical review.
Receipt of the elevated blood test results for the heart attack marker Troponin T, which had been ordered by the ED nurse, was also delayed as there was no clear process for escalating nurse-ordered tests to the patient’s doctor, surgical registrar ‘Dr A’. The combination of busyness, the six-hour ED target, delayed medical review and late receipt of the Troponin T results meant Mr B’s planned transfer to a surgical ward was carried out by ED nursing staff when, in retrospect, his signs of sepsis and a heart attack meant he should have been considered for higher level care (though no beds were available in either the ICU or coronary care unit at the time of his admission).
The HDC heard that that it was not unusual for the surgical team to fail to complete ED-to-ward bed request transfer forms, which were left for the ED nursing staff to do instead. Hill said he was critical that the DHB’s ward transfer practice did not match its policy, which would have required that Dr A, rather than nursing staff, complete the bed request form (see case summary below for more details).
Among a number of recommendations made by the commissioner was for the DHB to audit the new triage process it had since introduced; for the DHB to develop a clear policy for who is responsible for following up test results ordered by ED registered nurses; and for it to remind all ED staff that a patient transfer and location must be “clinically appropriate”.
Other recommendations included that the DHB review its sepsis management policy and adult sepsis pathway (and provide training for relevant staff on the new pathway); consider implementing a system that requires the laboratory to alert the patient’s treating clinician urgently; review the ED’s standard operating procedure; develop a care escalation plan for the general medicine team; and review the role of on-call consultants to ensure that adequate supervision of junior doctors is occurring. In addition, he requested that the DHB send a written apology to Mr B’s family.
The DHB told HDC that since the 2014 event “significant changes” to its ED triage process had been made, including building a new triage area that allows a patient to be seen by a triage nurse in a private area. In addition, the number of medical registrars available to see acute patients in the ED had been increased from one to two during the busier parts of the day and it now had an Adult Sepsis Pathway for ED. A new ED treatment chart with space allocated specifically for detailing by nursing staff of the blood tests they had ordered had also been developed.
CASE HISTORY SUMMARY
‘Mr B’ was first admitted to the hospital’s surgical ward a week before his death with a four-week history of diarrhoea and abdominal pain.
Mr B was discharged as surgical staff thought his symptoms, which included variable temperatures and a borderline elevated white cell count, were due to his gout medication, but a plan was put in place for an urgent outpatient colonoscopy.
On Day 8 Mr B’s GP phoned the surgical registrar Dr A as Mr B was still unwell, and Dr A accepted him for review in the ED.
Mr B walked into ED just before 10am and was triaged by an RN 35 minutes later on a particularly busy day with a ‘Code Orange’ being called at 10.30am. He was given a triage score of three. At 10.50am Mr B was given an initial review by Dr A, who gave a provisional diagnosis of abdominal sepsis. He requested a medical review by medical registrar Dr D, but Dr D was very busy with the influx of patients.
Nurse E started IV fluids and at 11.20am requested several routine blood tests, including a Troponin T test, because of the patient’s heart history, but this was not recorded on the patient’s ED clinical record. She told HDC that regrettably an ECG was not completed but she was not focused on a complete cardiac work-up, given Mr B’s repeat referral to the surgical team and his presenting symptoms suggesting a gastric condition. The DHB said it was usual practice for ED nurses to initiate blood tests and nurses were not responsible for viewing or acting on the results but were expected to indicate which tests were ordered on the ED clinical record.
At 11.40am Nurse E recorded that the plan was to admit Mr B to the surgical ward. The abnormal Troponin T results were reported by the lab at 12.13pm, but there was no automatic process for alerting Dr A and he told HDC that as he was unaware they had been ordered he did not look out for the results or chase them up.
Dr A reviewed Mr B for a second time when he was halfway through his first bag of IV fluid and noted he was responding to the treatment but was still sleepy. At 1.20pm RN E recorded that Mr B was transferred to a room closer to the desk because of his low blood pressure. At 1.53pm she completed an ED to Ward bed request form for the surgical ward, based on his GP referral to the surgical team, his gastric symptoms and his recent admission to the surgical ward.
At 2.35pm Dr A viewed Mr B’s blood test results, including the Troponin T result, which indicated sepsis and heart damage. He spoke to medical registrar Dr D again, who said he would review Mr B soon but was still busy.
Mr B was transferred to the surgical ward shortly before 3pm without blood cultures having been taken, a catheter inserted, a catheter specimen of urine taken, a fluid balance chart commenced, stool cultures taken, or an ECG undertaken.
RN E told HDC that starting a fluid balance chart would have been ideal practice, but it was exceptionally busy that day and it was not unusual for care plans not to be fully completed in ED. “In the turmoil of a stressed ward, completing tasks, procedures and paperwork becomes a juggle whilst prioritising patient care,” she said.
By the time Dr D went to review Mr B, he had been transferred to the surgical ward, so he went there and carried out a review (about four and a half hours after medical review was first requested) and put in a management plan.
Dr A prescribed Mr B antibiotics at approximately 3pm. Between 3pm and 4.25pm, Mr B underwent an ECG, chest X-ray, and medical review. Sadly, Mr B’s condition deteriorated and he died at 5.17pm.
A subsequent post-mortem examination showed infective endocarditis of the aortic valve involving adjacent heart tissue, fibrinous pericarditis and evidence of heart failure. Death was considered to be due to infective endocarditis.
The full report can be viewed here
]]>
Jen Gow, the Southern DHB’s Releasing Time to Care charge nurse manager, said its Sit Up, Get Dressed and Keep Moving initiative would encourage patients to get dressed and moving as quickly and as safely as possible to avoid the potential negative impacts of being bed-bound.
She said the Southern campaign was aimed at supporting patients of all ages and particularly encouraging and reassuring older people it was okay to wear clothes and walk around.
“For an older patient the effect of being in a hospital bed can be far-reaching,” said Gow. She said unnecessary bed rest could lead to reduced muscle strength, increased risk of falls, reduced mobility and loss of confidence. This could delay to delays in re-establishing normal routines and older people being able to return home.
Gow said Dolan would be running a workshop for health professionals and colleagues from across the Southern health system next week in Dunedin. Dolan is director of service improvement at Canterbury District Health Board but spends about four months of the year in the UK as a consultant and an honorary and visiting professor at two UK institutions.The workshop will be based on Dolan’s TODAY model for change programme.
Southern DHB’s new Chief Nursing & Midwifery Officer Jane Wilson said Dolan’s message was clear that patient time was the “most important currency in healthcare” and this was supported by the DHB.
Sit Up, Get Dressed, and Keep Moving was being launched today by the DHB, with displays in the foyers of Dunedin and Southland Hospital and information in the hospital wards through posters and leaflets to educate staff, patients and visitors.
The #endPJparalysis movement started early this year as a twitter hashtag linking twitter conversations on the topic of getting older patients up and dressed. The West Coast DHB was the first DHB to get behind the movement, with medical ward clinical nurse manager Rose Kennedy saying it provided a framework for medical wards like her own to support a restorative model of care and hadn’t added to the nursing workload, just reshaped it.
]]>
Lesley Harry, NZNO industrial advisor, said a second facilitated forum was being held today on addressing chronic understaffing and implementing the safe staffing Care Capacity Demand Management (CCDM) tools with DHB, Ministry of Health and New Zealand Nurses Organisation representatives
Chief Nursing Officer Dr Jane O’Malley confirmed she is attending the meeting on how to hasten the roll out of CCDM as the Ministry’s executive representative and as “an observer and support”.
Harry said today’s (16 August) CCDM safe staffing forum was a follow-up to an earlier forum held on July 18 to help inform the multi-employer collective (MECA) negotiations which got underway between the DHB and NZNO in June.
During the 2015 negotiations the DHBs ‘reaffirmed’ their commitment to implementing the safe staffing CCDM system* including making a ‘timely response’ when CCDM analysis showed that more nursing positions were needed to meet patient acuity and demand trends. But by midway through this year only 14 DHBs were underway with implementing CCDM and few had completed full implementation.
Harry said in negotiations earlier this month NZNO had reiterated issues relating to its pay equity claim and intended to discuss Australian comparators when negotiations resumed on August 23.
In early August NZNO negotiators had also held discussions with DHB directors of nursing over plans for registered nurse (RN) prescribers and how the RN prescriber role might fit into the current employment agreement’s senior nurse framework.
The MECA negotiations cover about 27,000 registered nurse, enrolled nurse, midwife and health care assistant members of NZNO. The current MECA expired on 31 July.
In its latest MECA bargaining update the NZNO said it had also agreed to refer discussions about support for victims of domestic and family violence to a joint forum on 5 September with fellow health unions, the Public Service Association (PSA) and E tū.
*CCDM three core components
- Mix and Match Staffing (i.e. using patient acuity data analysis to calculate the safe FTE base staffing required for a ward or unit to meet patient demand patterns)
- Variance Response Management (i.e. capacity at a glance screen (CAG) and ‘traffic light’ system to alert when ward is in immediate need and systems of how to respond)
- Core data set (Using high-quality data to review and respond to safe staffing needs)
CCDM DHBs (at various stages of implementation)
- Bay of Plenty
- Northland
- MidCentral
- Nelson
- Tairawhiti
- Taranaki
- Southern
- Waitemata
- Hutt Valley
- Whanganui
- South Canterbury
- Auckland
- Hawke’s Bay
- Capital & Coast
Have validated patient acuity system and CCDM under discussion
- Wairarapa
- West Coast
Progressing validation of another patient acuity system
- Counties Manukau
- Waikato
Considering acuity system options
- Canterbury
- Lakes
Building work will begin this year and the expansion is expected to be completed by next winter, allowing nearly 100 additional complex surgeries per year. The unit currently has around 1,500 ICU admissions each – more than half from other DHBs around the lower North Island and upper South Island.
]]>