A recent review of the National Bowel Screening Programme (NBSP) raised concerns about the capacity and fragility of the colonoscopy workforce.
Professor Gregor Coster, the review chair, said the colonoscopy workforce capacity remains a significant risk and is constraining the current NBSP roll-out.
In 2014 the National Nurse Endoscopy Advisory Group was established to develop and implement endoscopy nursing roles to help meet the expected workforce demands of the bowel screening programme.
Implementing the training programme to meet the demands for this new workforce, while being able to meet the targets set for the National Bowel Screening Programme, has not been without its challenges. Some of those we have faced and conquered, while some are still being addressed.
One of these challenges is that DHBs have to demonstrate a level of organisational readiness to be able to support nurses to complete the nurse endoscopy training and credentialing programme. The training programme needs not only nurses who have met the academic and clinical practice prerequisites but also the endorsement by DHBs of nurses performing endoscopies and a plan for the execution of the programme in accordance with the Nursing Council of New Zealand’s guidelines for the expanded practice for registered nurses.
The first priority for credentialed nurse endoscopists will be to provide routine endoscopies, which will free up experienced endoscopists to carry out bowel screening colonoscopies.
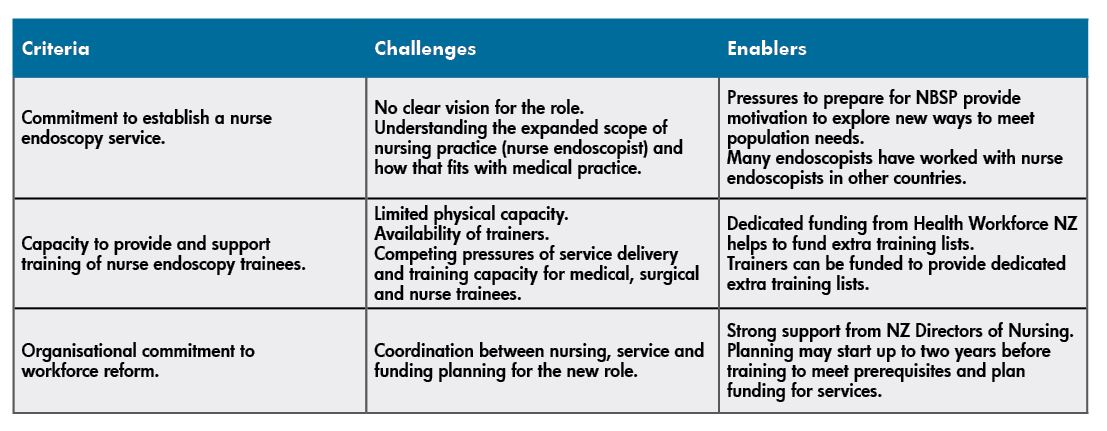
The criteria for determining DHB readiness are discussed in the table below, where we look at the particular challenges we have faced, and are still currently facing, in the ongoing delivery of the endoscopy training programme.
Delivery of the inaugural nurse endoscopy training programme got underway at the University of Auckland in 2016 as part of the Health Workforce New Zealand initiative to introduce the role of the nurse endoscopist.
The first cohort of four candidates has successfully completed the one-year academic programme (plus over 200 scopes each) and all have been accredited in at least one of the three scope modalities: gastroscopy, flexible sigmoidoscopy and colonoscopy. It takes at least two years of supervised training for any endoscopist trainee to reach competence, with the timing varying on their access to training lists and individual ability.
The challenges mentioned earlier meant there was no cohort in 2017, but a further four candidates started the academic programme this year and it is hoped to have four students in 2020. DHBs still have many questions about how to prepare for nurse endoscopists and part of our role has been to coach and support DHBs in introducing the new role.
Geographically, the students are from Auckland, Waikato and Otago, with five DHBs – Auckland, Counties Manukau, Waitemata, Waikato and Southland – currently engaged in the programme. There is growing interest from other DHBs, which is promising.
Nurse endoscopists have the potential to work across the continuum of care and this is already becoming evident, with two of the candidates from the inaugural course completing their prescribing pathway; one following the RN designated prescriber pathway and the other on the nurse practitioner pathway.
Collaborative curriculum
The University of Auckland developed the curriculum in collaboration with clinical experts to provide the theoretical and clinical skills component.
The academic component of the programme includes two postgraduate courses at master’s level completed in one academic year. To join the programme, nurses must have a clinical postgraduate diploma and a minimum of five years’ clinical experience post-registration. Three of those years are required to be in gastroenterology/endoscopy or a related specialty area such as colorectal surgery.
The endoscopy training programme focuses on the ongoing development of clinical expertise, using a practice development approach emphasising person-centred, evidence-based practice and critical thinking skills to improve health outcomes.
The clinical course coordinator of the endoscopy programme plays a crucial role, using knowledge of the sector to work with DHBs and clinicians to support trainees. Work-based training starts alongside the academic programme to allow the integration of increasing theoretical knowledge with practical skills.
Training continues until competence is achieved against an independent set of criteria aligned to national standards set by the Endoscopy Guidance Group of New Zealand (EGGNZ) for performing bowel screening colonoscopies. These standards apply to all endoscopists, whether they are medical practitioners or nurses.
The first priority for credentialed nurse endoscopists will be to provide routine endoscopies, which will free up experienced endoscopists to carry out bowel screening colonoscopies.
The academic/clinical partnership was critical when it came to working with the national steering group and setting the expectation that nurses provide both clinics and endoscopy lists to ensure holistic practice and the development of assessment and diagnostic skills.
The nurse endoscopy candidates are encouraged to spend time with areas aligned to the service to develop networks and gain a wider knowledge of pathology, radiology, surgery and multidisciplinary meetings. We have also worked with DHBs to develop standing orders as the sedation drugs commonly used during endoscopy are not currently on the list of drugs available to designated nurse prescribers. The support from anaesthetists in providing theoretical and simulation training has also been appreciated and is ongoing as we plan for changes at a national level to support this new role.
We have worked closely with DHBs and interested nurses to ensure they are ready before starting their journey. It has been a pleasure and a privilege to work with a wide range of people to overcome barriers when implementing this new role and delivering services to patients in a new way.
It is humbling to witness the personal and professional growth of students as they undertake the endoscopy training programme and lead the way for the future nursing workforce.
About the authors: Lesley Doughty RN MEd (Hons) (PG Programme Director) and Jacky Watkins RN MN (Course Coordinator) are professional teaching fellows at the University of Auckland and are responsible for developing and implementing the nurse endoscopy training programme.





















