This learning activity is relevant to the Nursing Council registered nurse competencies 1.1, 1.4, 2.1-2.4, 2.6, 2.8-2.9.
Learning outcomes
Reading and reflecting on this article will enable you to:
- further your understanding of how the quality of clinical service delivery is measured in your workplace
- review your understanding of skin tear injuries and their significance for the individual concerned.
Introduction
Henry had been living in an aged residential care facility for several years. He was now frail and confused, requiring assistance with almost all aspects of daily living. Paul, Henry’s son, visited him at least twice weekly, and on a recent visit noticed that his lower arm was bandaged. Staff were unable to tell Paul what had happened to Henry’s arm, and there was no wound assessment or treatment plan. According to the wound register, Henry had two other skin tears on his legs, but the status of these wounds was unclear.
When the registered nurse removed Henry’s arm bandage, two large and inflamed skin tears (each with a partial flap loss) were found. Skin closure strips had been used on both injuries and then covered with dry dressings, which had adhered to the wounds. Henry moaned loudly and kept trying to move his arm away when the areas were being redressed1.
Although skin tears represent more than half of all skin injuries in older adults, they have been described as forgotten wounds2, receiving little attention or research.
Skin injuries such as skin tears are often regarded as inevitable, and remain underappreciated, under-reported and essentially invisible3. Yet nurses working with older adults in all clinical settings are likely to encounter skin tears on a very regular basis.
The factors that contribute to the quality of nursing service delivery for older adults are complex, and singling out just one measure alone cannot offer a valid representation of the quality of service delivery. However exploring events and injuries such as skin tears in more depth enables clinical staff and management to identify opportunities for improving service delivery and reducing potential/actual distress and injury for older adults.
Skin tears revisited
Skin tears are “wounds caused by shear, friction, and/or blunt force, resulting in separation of skin layers. A skin tear can be partial thickness (separation of the epidermis from the dermis) or full thickness (separation of both epidermis and dermis from underlying structures)”4. (Refer to the STAR Skin Tear Classification System [see Box 1 Next page]5 and the learning activities associated with this article for further information on skin tear classifications and management). Although there are a number of commonly recognised classification tools for assessing and documenting skin tears, international research suggests these are not used regularly6.
Internationally, information on the skin tear prevalence and incidence rates are limited2. It has been suggested that under-reporting occurs because of a primary focus on pressure injuries, and that iatrogenic skin injuries, such as skin tears, and incontinence-associated dermatitis, are regarded as an inevitable part of ageing3. The New Zealand prevalence rate (number of new and current skin tears) is unknown7.
ACC accepts claims for primary injuries that include skin damage, injury or tears related to treatment by a registered health practitioner, but it cannot provide data specific to skins tears. Between 2011 and 2016 the number of accepted treatment-related claims for skin damage, injury or tears varied between 161 and 239 per year, with an average of 181 claims per year.
Since data was collected in 2005, 79 per cent of accepted claims for this primary treatment injury relate to individuals aged over 65 years of age. Nursing is the lead ‘context’ of these injuries and the top three treatment events that resulted in the injury are firstly removal of dressings/wound care; secondly patient transfer, and lastly removal of strapping8.
Australian researchers identified an incidence rate of 10.6 per 1,000 occupied bed days in their control group of residents in aged care facilities, while another study identified a 20 per cent prevalence rate in adults aged over 80 years living in the community9.
The skin of older adults is particularly vulnerable to injury, and iatrogenic skin injuries result from complex, multifactorial and interconnected threats3. Tissue tolerance is affected by:
- advancing age
- pre-existing health status and comorbidities
- level of nutrition
- medications
- perfusion
- oxygenation
- mobility
- sensory perception3.
Environmental factors, such as staff turnover, skill mix, and knowledge and care practices all have the potential to exacerbate skin tear rates.
Skin tear outcomes
Skin tears range from relatively minor to extensive and complex wounds, although they may be perceived by some as minor injuries10. Like any wound, they are a potential site of infection, especially in the frail elderly, as well as impacting on the person’s quality of life. Skin tears can be painful, as the superficial nerve endings are usually affected10 and have the potential to become chronic wounds.
The management of skin tear injuries further adds to staff workloads and care delivery costs. When older adults experience skin tears on a regular basis, keeping track of multiple injuries and their healing status can prove challenging. This is especially so when these wounds may not require daily changes of dressing if appropriate dressings are used, meaning there is an increased potential for them to be overlooked.
The experience of a skin injury, such as a skin tear, is unique and specific to each individual injury, and can impact on all aspects of the person’s wellbeing3. Ongoing skin tears can be a very visible and unwelcome reminder for both individuals and their families of physical deterioration. When a person experiences multiple skin tears over time, they also have the potential to cause family members to question the quality of service delivery.
BOX 1
STAR Skin Tear Classification System Guidelines
- Control bleeding and clean the wound according to protocol.
- Realign (if possible) any skin or flap.
- Assess degree of tissue loss and skin or flap colour using the STAR Classification System.
- Assess the surrounding skin condition for fragility, swelling, discolouration or bruising.
- Assess the person, their wound and their healing environment as per protocol.
- If skin or flap colour is pale, dusky or darkened reassess in 24-48 hours or at the first dressing change.
STAR Classification System
1. Category 1a
A skin tear where the edges can be realigned to the normal anatomical position (without undue stretching) and the skin or flap colour is not pale, dusky or darkened.
2. Category 1b
A skin tear where the edges can be realigned to the normal anatomical position (without undue stretching) and the skin or flap colour is pale, dusky or darkened.
3. Category 2a
A skin tear where the edges cannot be realigned to the normal anatomical position and the skin or flap colour is not pale, dusky or darkened.
4. Category 2a
A skin tear where the edges cannot be realigned to the normal anatomical position and the skin or flap colour is pale, dusky or darkened.
 5. Category 3
5. Category 3
A skin tear where the skin flap is completely absent.
From: STAR Skin Tear Classification Tool developed by Skin Tear Audit Research (STAR). Silver Chain Group Limited, Curtin University. Revised 4 February 2010. Reprinted August 2012. You can download full STAR tool and glossary at: www.woundsaustralia.com.au/wa/resources.php
Is our service up to standard?
Measuring the quality of care is a complex and multifaceted undertaking.
All healthcare services in New Zealand are regularly assessed against the Health and Disability Sector Standards (2008)11. Compliance with these standards includes having a plan for measuring the quality of services, which may involve monitoring quality indicators (see Box 2), complaints, service user satisfaction surveys, and responses to identified issues.
New Zealand’s Health Quality and Safety Commission12 has developed a set of quality markers that track progress over time in the health and disability sector relating to four key priority areas – falls, healthcare associated infections, surgical harm and medication safety.
A Standards New Zealand Working Party developed specific clinical indicators for individuals requiring aged care or dementia care in 2005 (see Box 2)13. Indicators include pressure injuries, falls, urinary tract infections and staffing hours but not skin tear rates. However, skin tear rates should be included as a clinical indicator for any organisation providing services to older adults because of the frequency of these injuries, their impacts on individuals, and the many opportunities for preventing/minimising their occurrences.
Monitoring skin tear injury rates provides a valuable overview of service delivery, while auditing individual cases (tracer methodology) offers a window into systems and processes. The Ministry of Health14 suggests that examining the journey of a specific client/resident/patient facilitates understanding of the care that is being provided and shows if staff know how to deliver care, tests systems and processes and their function and validates the individual’s journey and outcomes (p.4).
A detailed review of just one service user’s experience with a skin tear injury can provide a range of valuable information, including:
- wound management practices and consistency with service policies – systems and processes for assessing/classifying/evaluating and reporting on wound progress; evidence-based wound management practices (e.g. not using skin closures on skin tears15); use of appropriate wound care products; monitoring for infection; checking that wounds are regularly monitored until they heal
- assessment and care planning – short-term plans related to the skin injury and its associated clinical requirements, such as analgesia, enhanced nutrition; strategies to minimise risk of skin injuries or further injuries, such as avoiding soaps and using skin moisturisers twice daily9, and the use of appropriate transfer equipment, for example, slider sheets
- capturing relevant data – initial and ongoing documentation in the clinical record related to the injury; completion of an accident/incident report; open disclosure to the individual and/or family; analysis of incident and accident data; mechanisms for responding to findings, reporting results to staff, actioning any identified deficits.
In conjunction with reviewing individual cases, an analysis of skin tear injury rates across the service can tell us about environmental factors that may contribute to these injuries, such as the times of day the injuries occur; the skin tear site; staff skill mix and ratios; staff education and knowledge deficits. These are modifiable factors the organisation can work towards addressing.
BOX 2: Indicators for safe aged care
An indicator is a measure or flag against which some aspect of a standard can be assessed. Indicators generally simplify and quantify complex phenomena and aid the communication of information about those phenomena. Indicators are information tools. They summarise data on complex issues to indicate the overall status and trends on those issues. Indicators are generally measures that link the processes of care with desirable outcomes13 (p.13-14).
Conclusion
Unfortunately, skin tears are a common occurrence for many older adults, resulting in pain, distress, and the potential for chronic wounds. Skin tear injuries result from many interlinked factors relating to the individual, the environment, and care practices. Some of these factors are modifiable, such as patient handling procedures, and others, such as significant frailty, are not.
While it is important that skin tears are prevented when possible, and when they occur are carefully and appropriately managed using best practice, these injuries also offer a picture into the quality of care received by individuals and a patient cohort. Rather than being a forgotten and inevitable wound for older adults, skin tears should be a key reminder of the complexity of care for this growing population.
View the PDF of this learning activity here >>
About the authors:
- Lesley Batten RN PhD is a senior researcher at Massey University, Palmerston North.
- Marian Bland RN PhD is a healthcare auditor.
This article has been peer reviewed by:
- Julie Betts RN MN, who is a wound care nurse practitioner at Waikato District Health Board.
- Rebecca Aburn RN MN, who is an infection prevention and control nurse specialist at Southern District Health Board with a special interest in wound care.
Recommended resources
- The International Skin Tears Advisory Panel website includes a range of resources, including the Skin Tear Resource Kit, a skin tear decision algorithm, and consensus statements relating to the prevention, prediction, assessment and treatment of skin tears. www.skintears.org
- The New Zealand Health and Safety Commission website includes comprehensive information on evaluating health quality.
www.hqsc.govt.nz/our-programmes/health-quality-evaluation - Pharmac’s 2015 Seminar Series focusing specifically on wounds is available via You Tube. The first part of the fourth video in this series, titled From skin tears to leg ulcers, covers a range of information relevant to skin tear prevention and management.
www.youtube.com/watch?v=JKme8c9KyB4 - The Skin Safety Model proposed by Campbell, Coyer and Osborne offers a new perspective on older adults’ vulnerability to skin injuries and outlines a framework for skin care and the promotion of skin integrity. CAMPBELL J, COYER F & OSBORNE S (2016). The skin safety model: reconceptualising skin vulnerability in older patients. Journal of Nursing Scholarship 48(1) 14-22.
http://onlinelibrary.wiley.com/doi/10.1111/jnu.12176/full - Detailed information on the selection of wound products for skin tears can be found in the following article: LEBLANC K, BARANOSKI S & LANGEMO, D et al (2015) The art of dressing selection: a consensus statement on skin tears and best practice. Advances in Skin and Wound Care 29(1) 32-46.
- Information relating to the prevention of skin tears is outlined by: SUSSMAN G & GOLDING M (2011). Skin tears: should the emphasis be only their management?
Wound Practice and Research 19(2), 66-70.
References
- Personal anecdote as told to Marian Bland.
- LEBLANC K & BARANOSKI S (2014) Skin tears: the forgotten wound. Nursing Management 45(12) 36-46.
- CAMPBELL J, COYER F & OSBORNE S (2016) The skin safety model: reconceptualising skin vulnerability in older patients. Journal of Nursing Scholarship 48(1) 14-22. http://onlinelibrary.wiley.com/doi/10.1111/jnu.12176/full
- INTERNATIONAL SKIN TEARS ADVISORY PANEL (2015). www.skintears.org
- SILVER CHAIN GROUP & CURTIN UNIVERSITY (2007) STAR skin tear classification system. Retrieved from www.woundsaustralia.com.au/publications/2010_wa_star-skin-tear-tool-g-04022010.pdf
- HOLLISTER AND INTERNATIONAL SKIN TEARS ADVISORY PANEL (2013). Skin tear resource kit. www.skintears.org/pdf/Skin-Tear-Resource-Kit.pdf
- MILNER E (2013). Simple tear but complex wound. Nursing Review 13, 18-19. www.hqsc.govt.nz/assets/Falls/10-Topics/Milner-Nursing-Review-Nov-2013-Skin-tears.pdf
- ACC TREATMENT INJURY DATA FROM 1 JULY 2005. [Skin treatment injury data emailed by ACC to Nursing Review on 21 April 2017 following request for information.]
- CARVILLE K, LESLIE G, OSSEIRAN-MOISSON R, NEWALL N & LEWIN G (2014). The effectiveness of a twice-daily skin-moisturising regimen for reducing the incidence of skin tears. International Wound Journal 11, 445-53.
- STEPHEN-HAYNES J & CARVILLE K (2011). Skin tear made easy. Wounds International 2(4). Retrieved from www.woundsinternational.com/media/issues/515/files/content_10142.pdf
- MINISTRY OF HEALTH (2016a). Service standards. www.health.govt.nz/our-work/regulation-health-and-disability-system/certification-health-care-services/services-standards.
- HEALTH QUALITY AND SAFETY COMMISSION NEW ZEALAND (2016). Health Quality and Safety Indicators. www.hqsc.govt.nz/our-programmes/health-quality-evaluation/projects/health-quality-and-safety-indicators
- STANDARDS NEW ZEALAND AND MINISTRY OF HEALTH (2005) New Zealand Handbook – indicators for safe aged-care and dementia-care for consumers. SNZ HB 8163:2005.
- Ministry of Health (2014). Tracer methodology revisited. HealthCert Bulletin: Information for Designated Auditing Agencies 11, 4. www.health.govt.nz/system/files/documents/pages/healthcert-bulletin-11-april-2014.pdf
- LEBLANC K, BARANOSKI S & LANGEMO, D et al. (2015). The art of dressing selection: a consensus statement on skin tears and best practice. Advances in Skin and Wound Care 29(1) 32-46.
- NURSING COUNCIL OF NEW ZEALAND (2012) Competencies for registered nurses. Retrieved January 2016 from www.nursingcouncil.org.nz/Publications/Standards-and-guidelines-for-nurses
This learning activity is relevant to the Nursing Council competencies 1.1, 2.8, 2.9.
Learning outcomes
- Understand rationale for developing a nursing portfolio.
- Know how to approach a self-assessment against the competencies using everyday practice examples.
- Increase familiarity with the Nursing Council of New Zealand website.
- Locate and review guidelines that underpin nursing practice.
Introduction
“What is a portfolio? Is it a PDRP? Is it a massive file of information about your practice? How do I even begin to self-assess when the competencies aren’t specific? Anyway, this will take weeks to put together…won’t it? I am good at my job, WHY are you auditing ME?”
This article looks at why nurses need to develop a portfolio and offers advice on how to effectively self-assess nursing practice against the Nursing Council of New Zealand competencies if faced by a recertification audit.
There are two circumstances when nurses need to present a portfolio:
Being randomly selected for a recertification audit of the continuous competence requirements by the Nursing Council of New Zealand (NCNZ).
OR
Being employed by an organisation with an approved Professional Development and Recognition Programme (PDRP)8 and being required to submit a portfolio on a three-yearly cycle or wishing to apply for another level of practice. (Nurses on a PDRP should seek specific advice from their PDRP coordinator.)
Why portfolios?
The Health Practitioners Competence Assurance Act (2003)¹ provides a framework for the regulation of health practitioners to protect the public where there is risk of harm from professional practice. The Act identifies responsible authorities (e.g. NCNZ) that have the role of ensuring all registered health practitioners, issued with an annual practising certificate (APC), are competent in their scope of practice.
The Council has the role of protecting the public by setting standards and ensuring that nurses are competent to practise under the Act. Each year the Council randomly selects five per cent of practising nurses for a recertification audit14.
Question: When you receive your APC notification from NCNZ, do you tick the boxes that declare:
- you have the required 450 practice hours (over three years)?
- you have the required 60 professional development hours (over three years)?
- you are competent to practice?
Answer: Yes? Then the NCNZ recertification audit is asking you to provide validated evidence for those ticks.
TIPS BOX 1
- ONLY include the requested items from the checklist.
- Filling a portfolio does not need to be a linear process. Start with the items you already have.
- Write about your everyday practice, in your own words.
- This isn’t about your best day ever, it’s about what you do every day.
What is a portfolio?
A portfolio is a standardised way of storing information that describes your competence to practice. It’s generally an A4 folder, or an electronic equivalent, with predefined sections making it easier to collate and audit.
Filling a portfolio for recertification
Content
The NCNZ provide a checklist14 on their recertification webpage. Only include the items requested, keep it simple. Three forms of verified evidence are required:
- Record of practice hours.
- Record of professional development hours.
- Assessment against the competencies
- Self-assessment
- Senior nurse or peer review
Check the NCNZ website for templates7, 14, 15 and information. If you cannot meet one or more of the requirements, contact the NCNZ to explain your situation and they will advise you what to do.
Verification
The evidence you provide in your portfolio must be verified, which means signed by someone who has either observed your practice or can confirm that the evidence you have provided is correct and that it is your work. This is often a manager or senior nurse. They must provide their name, designation and contact details.
Currency
A portfolio is about your current practice. All the evidence/practice examples you provide must be from the previous three years.
Privacy
Any inclusion of third party information without consent is a breach of privacy3, 17.
Assessment against the RN competencies
Which competencies?
The majority of New Zealand’s approximately 50,000 registered nurses (RNs) are in ‘direct-care’ clinical roles16 and will complete the RN clinical competencies. However, there are nurses working across health in myriad different roles who do not provide direct nursing care but still influence nursing practice and/or the nursing workforce. The Council has created competencies to recognise and accommodate the breadth of the scope and RNs must select a competency set that reflects their current practice. There are competencies for RNs in:
- clinical⁴ (the majority of RNs)
- management6/clinical management⁶
- education6, policy6, and research6.
This article looks at the clinical competencies⁴ in the four domains:
- Domain 1: Professional responsibility (five competencies)
- Domain 2: Management of nursing care (nine competencies)
- Domain 3: Interpersonal relationships (three competencies)
- Domain 4: Interprofessional healthcare and quality improvement (three competencies)
Nurses must provide ONE practice example for every competency. Each competency has ‘indicators’ listed – these are guides to help you select your example.
TIPS BOX 2
- Put your practice examples into the domains then start with the competency you think is the easiest to describe. The indicators may help you decide.
- Write a statement about your practice then support it with an objective example (an actual situation that occurred).
- See the examples provided for the RN clinical competencies.
The RN domains and competencies with general examples and tips to guide you
Domain 1: Professional responsibility
Competency 1.1 Accepts responsibility for ensuring that his/her nursing practice and conduct meet the standards of the professional, ethical and relevant legislated requirements.
This covers legislation, acts, ethics, codes, policies and standards that underpin practice. e.g. Privacy Act, the Code of Rights and workplace health and safety requirements. Refer to the NCNZ Code of Conduct5 and other guidelines.
EXAMPLE for Competency 1.1
Statement about your practice:
We had a refresher on the NCNZ Code of Conduct, social media guidelines and professional boundaries last year (see PD hours), which was great, and we keep copies in the office. I am very aware of the Privacy Act, the patient’s right to confidentiality and how that affects who I can talk to about the patient
Actual practice example:
Last month I was caring for a gentleman whose neighbour rang to ask for results of a recent blood test; she said she was helping to care for him and he had asked her to call. I explained that I could not discuss the patient’s condition or blood tests because… etc.
Competency 1.2 Demonstrates the ability to apply the principles of the Treaty of Waitangi/Te Tiriti o Waitangi to nursing practice.
This is specific to Māori, in relation to the Treaty. How do you partner in care? How do you protect or advocate? How do you facilitate patient/whānau participation?10
Competency 1.3 Demonstrates accountability for directing, monitoring and evaluating nursing care that is provided by enrolled nurses and others.
Delegation occurs up, down or sideways e.g. asking a colleague for help (sideways), escalating a difficult situation to a manager (up), directing a student, healthcare assistant (HCA), or a patient’s family or carers (down). Refer to the NCNZ Direction and Delegation Guidelines12, 9.
Competency 1.4 Promotes an environment that enables client safety, independence, quality of life, and health.
How do you promote a safe working environment? How do you anticipate and mitigate clinical risk? How do you promote patient wellbeing and safety e.g hazard identification, reporting incidents, infection control guidelines?
Competency 1.5 Practises nursing in a manner that the client determines as being culturally safe.
How do you care for patients who have different cultural¹⁴ requirements from your own? How do you ascertain their beliefs and how you do respond? How do you know if the patient determines your care is culturally safe? Think broadly and beyond ethnicity. Culture includes many things that are part of our everyday lives e.g. religion, disability, sexuality, beliefs, food, family culture and language.
Domain 2: Management of nursing care
Competency 2.1 Provides planned nursing care to achieve identified outcomes.
How do you plan care? Do you use nursing models of care? Consider how you plan for an acute episode or a chronic illness, long term or short term. Who do you involve in the planning?
Competency 2.2 Undertakes a comprehensive and accurate nursing assessment of clients in a variety of settings.
How do you conduct your assessments? Do you use an assessment framework e.g. SOAP (subjective, objective, assessment, plan), mini-mental state examination, falls risk, InterRai? This could be initial assessment or assessment following a procedure, new medication or a regular reassessment. Consider how often you assess; you may have noticed something using your observation skills that prompted you to undertake a more focused assessment.
EXAMPLE for Competency 2.2
Statement about your practice:
We see walk-in patients and also take phone calls from patients. We need to be able to quickly assess in a variety of ways.
Actual practice example:
Walk-in: Last week a new patient presented with chest pain. As he came through the door I saw he was pale and sweaty, rubbing his chest. I immediately used the OLD CARTS chest pain assessment tool … etc.
Phone call: A young mum rang about her child who had a fever of 38.8 and had been unwell overnight with an ‘odd’ cough’. I used the Traffic Light System to identify the immediate risks: I asked for the child’s colour, activity … etc.
Competency 2.3 Ensures documentation is accurate and maintains confidentiality of information.
How do you maintain clear, concise, organised and current documentation?
EXAMPLE for Competency 2.3
Statement about your practice:
I document as soon as possible after a patient interaction; I always write things down in accurate detail as soon as I can with a time, date and signature, and then print my name.
Actual practice example:
About eight months ago a visitor made a complaint, claiming I gave their elderly relative the wrong advice about a medication. My manager checked back into the patient’s notes and I had written the conversation down in detail, timed and dated it, with a note that I had confirmed everything with the patient … etc.
Competency 2.4 Ensures the client has adequate explanation of the effects, consequences and alternatives of proposed treatment options.
How do you describe and explain a treatment, medication or a procedure to the patient? Do you encourage questions? Do they need a support person/interpreter/family member? Do you describe the alternatives and possible outcomes? Do you use printed information?
Competency 2.5 Acts appropriately to protect oneself and others when faced with unexpected client responses, confrontation, personal threat or other crisis situations.
What systems does your workplace have for crisis situations and what is your role in managing these? For example, cardiac arrest, security threat, anaphylaxis and other significant events.
Competency 2.6 Evaluates client’s progress toward expected outcomes in partnership with clients.
How do you assess if your care is safe and effective? How have you involved patients in care planning? How do you contribute to discussions and planning for the patients?
EXAMPLE for Competency 2.6
Statement about your practice:
I regularly meet with patients (and, if appropriate, their families) to discuss their requirements and preferences for their care.
Actual practice example:
I care for an elderly gentleman who is now unable to attend appointments for wound care because of chronic pain, transport issues and living alone. I recently organised to meet with him to review the options for his situation so he could get the care he needed in a way which met his planned care needs and his preferences starting with… etc.
Competency 2.7 Provides health education appropriate to the needs of the client within a nursing framework.
Why is health education important and how do you ensure you are offering it in a timely, consistent and appropriate way? Do you use printed resources or websites? Is it age and ability appropriate e.g. quit smoking, green prescription or a new medication? It could be to a patient, family or caregivers. How do you evaluate the effectiveness of your education?
Competency 2.8 Reflects upon, and evaluates with peers and experienced nurses, the effectiveness of nursing care.
How do you support your colleagues and peers to reflect on their practice? Does your employer have a system for seeking advice or debriefing? Have you made changes to patient care following reflection or professional discussion? Do you attend professional supervision?
Competency 2.9 Maintains professional development (PD).
You should include your PD record, but you can always add a reflection on a specific PD activity and how it affected your practice.
Domain 3: Interpersonal relationships
Competency 3.1 Establishes, maintains and concludes therapeutic interpersonal relationships with client.
It’s all about communication. How do you approach people every day; new patients or patients you have known for a long time? How do you form trusting relationships quickly and how do you maintain your longer term professional relationship with patients? How do you demonstrate knowledge of verbal and nonverbal skills (body language) in your communication with patients?
Competency 3.2 Practises nursing in a negotiated partnership with the client where and when possible.
Consider the patient’s right to refuse treatment – do you practice informed consent? How will the planned care work for the patient e.g. can they get to an appointment? What do you discuss with the patient to get the care they need in the right way, at the right time and place?
Competency 3.3 Communicates effectively with clients and members of the health care team.
Consider the many techniques you use to communicate with patients and to the team. How do you know they are effective?
EXAMPLE for Competency 3.3
Statement about your practice:
I think communication and listening is key to good practice. I always assess carefully when I meet patients to find out how they need to communicate and what works best for them.
Actual practice example:
Recently a new resident, an elderly gentleman who is profoundly deaf, had staff shouting instructions to him. I felt this undermined his dignity and was ineffective. I introduced myself to him and asked if I could sit next to him. I asked him if I could use a pen and paper to get my messages across in writing which he really liked … etc.
Domain 4: Interprofessional healthcare and quality improvement
Competency 4.1 Collaborates and participates with colleagues and members of the healthcare team to facilitate and coordinate care.
This is about the wider team, sometimes outside your own organisation. How do you work with other providers? How do you approach handover, multi-disciplinary meetings or case reviews? How do you organise a referral e.g. to a dietician or podiatrist, or discuss and plan care with other members of the healthcare team?
Competency 4.2 Recognises and values the roles and skills of all members of the healthcare team in the delivery of care.
Do you recognise when different skills are needed e.g. a physiotherapist, a social worker, a doctor? How do roles and clinical skills differ? How do you recognise and coordinate this e.g. in a discharge plan, patient deterioration, coordination of a procedure or appointment?
Competency 4.3 Participates in quality improvement activities to monitor and improve standards of nursing.
This could be participation in a clinical audit, survey, or nursing care quality initiative e.g. procedure technique, wound dressing, medication administration, documentation or communication process. Hazards, unsafe equipment or incident reporting. Focus on nursing practice.
Conclusion
In conclusion, a portfolio does not need to be confusing. Just step back, reflect on your practice and start recording your examples, competency by competency.
About the author:
- Liz Manning, RN, BN, MPhil (Nursing), FCNA(NZ) is a director of Kynance Consulting and is a nurse consultant who has worked in the area of portfolios, assessment, auditing and PDRP for many years.
This article was peer reviewed by:
- Linda Adams RN PG Cert HSc is a quality advisor for MedScreen. She is a former PDRP nurse advisor, recertification and PDRP auditor and competence assessor for NCNZ.
- Lorraine Hetaraka-Stevens RN PG Dip (nursing), MNurs (in progress) is an experienced competence assessor and nurse leader who is currently nurse leader of the National Hauora Coalition.
View PDF of this learning activity here >
REFERENCES
- HEALTH PRACTITIONERS COMPETENCE ASSURANCE ACT (2003). Retrieved December 2016 from www.legislation.govt.nz.
- MANNING L (2015). Tips for a top nurse portfolio. Nursing Review 15(2) 28.
- NEW ZEALAND NURSES ORGANISATION (2016). Guideline: Privacy, Confidentiality and Consent in the Use of Exemplars of Practice, Case Studies, and Journaling, 2016.
- NURSING COUNCIL OF NEW ZEALAND (2007). Competencies for Registered Nurses. Wellington: Author.
- NURSING COUNCIL OF NEW ZEALAND (2012). Code of Conduct. Wellington: Author.
- NURSING COUNCIL OF NEW ZEALAND (2011). Competence Assessment Form for Registered Nurses in Clinical Management. Competence Assessment Form for Registered Nurses Practising in Education. Competence Assessment Form for Registered Nurses Practising in Management. Competence Assessment Form for Registered Nurses Practising in Policy. Competence Assessment Form for Registered Nurses Practising in Research.
- NURSING COUNCIL OF NEW ZEALAND (2014). Examples for self-assessment and senior nurse assessment for the registered nurse scope of practice.
- NURSING COUNCIL OF NEW ZEALAND (2013). Framework for the approval of professional development and recognition programmes to meet the continuing competence requirements for nurses. Wellington: Author.
- NURSING COUNCIL OF NEW ZEALAND (2011). Guideline: Direction and Delegation of Care by a Registered Nurse to a Health Care Assistant.
- NURSING COUNCIL OF NEW ZEALAND (2011). Guidelines for Cultural Safety, the Treaty of Waitangi and Māori Health in Nursing Education and Practice. Wellington: Author.
- NURSING COUNCIL OF NEW ZEALAND (2012). Guidelines: Professional Boundaries. Wellington: Author.
- NURSING COUNCIL OF NEW ZEALAND (2011). Guideline: Responsibilities for Direction and Delegation of Care to Enrolled Nurses.
- NURSING COUNCIL OF NEW ZEALAND (2012). Guidelines: Social Media and Electronic Communication. Wellington: Author.
- NURSING COUNCIL OF NEW ZEALAND Recertification Audits & Recertification Audit Checklist.
- NURSING COUNCIL OF NEW ZEALAND (2011). Template for Evidence of Professional Development Hours.
- NURSING COUNCIL OF NEW ZEALAND (2015). The New Zealand Nursing Workforce: A Profile of Nurse Practitioners, Registered Nurses and Enrolled Nurses 2014–15. Wellington: Author.
- PRIVACY ACT (1993). Retrieved December 2016 from www.legislation.govt.nz/act/public/1993/0028/latest/DLM296639.html.
This learning activity is relevant to the Nursing Council competencies 1.1, 1.4, 2.1, 2.8, 2.9, 4.1, 4.2 and 4.3.
Learning outcomes
- Recognise the signs and symptoms of phlebitis.
- Summarise the distinguishing features of the four types of phlebitis.
- Take appropriate action to reduce the risks of phlebitis.
- Identify the risk factors and potential causes for IV cannula complications.
- Reflect on improvements that can be made to nursing practice to reduce IV complications.
Introduction
“Sam” (64) was admitted for elective surgery on his shoulder. He had had a few PIVCs during his admission. Medication from one of these cannulae (in his forearm), had infiltrated the surrounding tissue and the tissue then became necrotic. He required grafts and further surgery. This became infected. The infection went to his shoulder and he required further washouts of his shoulder1.
Insertion of a PIVC is one of the most common invasive clinical procedures performed in hospitals globally2 yet nurses are still not observing, assessing nor documenting the state of these regularly enough to reduce the risk of complications to the patient. PIVCs provide direct access into the venous system. Nurses must ensure that their knowledge and skills are up to date and based on current evidence-based practice to reduce the risk of patients with PIVCs preventing complications3.
Phlebitis
Phlebitis is one of the main complications from PIVC, with research indicating that the incidence can vary widely from less than 3 per cent up to more than 65 per cent depending on the clinical setting. This broad range suggests poor identification of phlebitis or poor reporting protocols4.
Phlebitis is defined as inflammation of the tunica intima or inner layer (see Fig. 1) of the vein, characterised by pain, redness and swelling5. The area may feel warm with a cord-like appearance of the vein and the patient may feel pain or discomfort when medication is administered.
There are four main types of phlebitis.
Chemical phlebitis is caused by fluid or medication being infused through the cannula. Key factors such as pH and osmolarity (the concentration of a solution) are known to have an effect on the incidence of phlebitis6. Blood has a pH of 7.35-7.45. Medications outside this range have the potential to damage the tunica intima (Fig. 1), the delicate inner layer of the vein (see Fig. 1), increasing the risk of patients developing phlebitis. This increases the risk of further injury to the vein, such as sclerosis, infiltration or thrombosis7.
Mechanical phlebitis happens when there is movement of the PIVC within the vein causing inflammation. This can be due to unskilled insertion or with placement of the cannula near a joint or venous valve, poorly secured cannulae, and manipulation of the cannula during administration of medication or fluid8. Having an insecure PIVC increases the risk of mechanical and infective phlebitis, with movement of the cannula causing migration of bacteria into the vein9.
Infective phlebitis is caused by bacteria entering the vein. Inflammation of the vein may begin as a non-infectious process caused by manipulation of the cannula or irritation from an infusion. Both chemical and mechanical phlebitis can produce inflammatory debris, which may serve as a culture medium for micro-organisms to multiply10. Once bacteria come into contact with the PIVC, they secrete a glue-like substance that causes the bacteria to stick to the plastic. This slimy protective substance is called biofilm. Antibiotics and white blood cells can’t penetrate this layer to kill the bacteria. Flushing and infusions can cause the biofilm to break off and travel into the patient’s bloodstream, with the associated risk of bacteraemia11.
Post-infusion phlebitis is an inflammatory response occurring after a PIVC has been removed. While most low-grade phlebitis will resolve when the cannula is removed, phlebitis may occur up to 48 hours later, with some evidence of occurrence up to 96 hours later8.

The Infusion Therapy Standards of Practice12 published in 2016 by the Infusion Nurses Society (INS), highly recommends the use of a phlebitis scale that is valid, reliable and clinically feasible; for example, the Jackson VIP Scale (Fig. 2). Intravenous Nursing New Zealand13, supports the use of the Infusion Therapy Standards of Practice to promote a consistent approach to catheter management when monitoring phlebitis. Interestingly, a systematic literature review published in 201414 identified more than 70 different phlebitis assessment scales in use worldwide. Nurses still need to be aware of the treatment required for the different types of phlebitis.

Management of phlebitis
Nurses should determine the possible aetiology of the phlebitis as noted below; apply a warm compress; elevate the limb; provide pain relief as needed; consider other pharmacologic interventions, such as anti-inflammatory agents; and use a visual scale, like the Jackson VIP Scale (Fig. 2), to consider whether removal (resiting) of the cannula is necessary10, 11. For example, if two of the following three are evident: pain near the IV site, erythema or swelling, no matter what the aetiology of the phlebitis, the PIVC must be removed and resited.
Chemical phlebitis: evaluate the infusion therapy and need for different IV access (e.g. central venous access device), different medication, or a slower rate of infusion; determine if removal of the PIVC is needed. Provide interventions as above10, 11.
Mechanical phlebitis: stabilise the IV cannula, apply heat, elevate the limb, and monitor closely. If signs and symptoms persist after 48 hours, consider removing PIVC as per Jackson VIP Scale (Fig. 2)10, 11.
Infective phlebitis: if suspected, (pain, erythema, swelling), remove the PIVC. Follow local policy regarding microbiology culture to identify the organism and incident reporting. Medical assessment will be required for the initiation of any antibiotic treatment. Monitor for signs of systemic infection10, 11.
Post-infusion phlebitis: if this appears to be a bacterial source, ensure that medical review is initiated, monitor for signs of systemic infection; if nonbacterial, apply warm compress, elevate limb, provide analgesics as needed, and consider other pharmacologic interventions. such as anti-inflammatory agents or corticosteroids as necessary10, 11.
Reducing the risks of phlebitis
Having a skilled practitioner or IV team inserting IV cannulae is proven to reduce many complications of PIVC15. IV teams are not always practical for all settings, but having skilled, trained IV practitioners who regularly update their skills and knowledge is a necessity for improving clinical quality and reducing risk. It has been demonstrated that skilled cannulators have a significantly higher first-time insertion rate, which is associated with a lower incidence of phlebitis and failure16.
Chemical phlebitis
- patients at risk may need to be referred for a central venous access device, such as a peripherally inserted central catheter (PICC) depending on the pH and tonicity of the medications to be administered7.
Mechanical phlebitis
- Prevent movement by carefully securing the cannula with a sterile, occlusive, transparent semipermeable polyurethane dressing9.
- Ensure the cannula hub is not directly accessed close to the insertion site9.
- Keep dressing dry and redress if the dressing loses its integrity.
- Select the smallest practical cannula for the largest possible vein.
- Avoid placing PIVCs near to joints i.e.
- ante-cubital fossa, to reduce irritation of the vessel wall by the tip of the cannula during movement6.
Infective phlebitis
As above (mechanical phlebitis), plus:
- Strict hand hygiene.
- Clipping excess hair from the preferred insertion site.
- Ensure strict aseptic non-touch technique during insertion of the cannula.
- Perform skin antisepsis with >0.5 per cent Chlorhexidine/70 per cent alcohol12, cleansing the skin with friction for 30 seconds and allow the solution to dry naturally. If a Chlorhexidine/alcohol solution is contraindicated, consider using povidone-iodine or 70 per cent alcohol wipes.
- No repalpating of the preferred site after cleansing.
- Use appropriate sterile IV dressing.
- ‘Scrub the hub’ of the needleless connector every time the cannula is accessed with single use disinfecting agent e.g. 70 per cent alcohol wipes or >0.5 per cent Chlorhexidine/70 per cent alcohol wipe, for at least 15 seconds12.
- Check the integrity of the PIVC dressing.
- Carefully remove the dressing that has lost its integrity and replace with new sterile dressing, taking care not to manipulate the sited cannula.
- Only use flush solutions from a single use system. Minimum of 10mL pre- and post-IV medication or according to local medication policy11.
Post-infusion phlebitis
A recent Australian study17 noted that the main predictor of post-infusion phlebitis was cannulae inserted under emergency situations, reinforcing the following recommendations:
- Replace all PIVC inserted under emergency conditions as soon as feasibly possible, i.e. within 24 to 48 hours12.
- Observe the insertion site for at least 48 hours after removal of the cannula.
- Educate the patient or family on discharge about signs and symptoms of phlebitis17.
Reducing the risk of other PIVC complications
Nurses also need to be cognisant of other complications leading to PIVC failure.
A quarter of PIVCs fail through accidental dislodgement or occlusion. Infiltration and extravasation (see Definitions box), haematoma formation or thrombophlebitis and septic thrombophlebitis may then occur18. It has been suggested that the use of visualisation devices (infrared or ultrasound) can increase the success of first-attempt insertion and decrease trauma to the patient19.
Good PIVC management
Early identification and intervention are critical to prevent serious adverse events, such as extensive tissue injury or nerve injury leading to compartment syndrome requiring surgical intervention20.
If a patient reports any burning or stinging at or around the insertion site or anywhere along the venous pathway:
- stop infusion immediately
- disconnect the IV tubing from the PIVC
- attempt aspiration of the residual medication from the cannula
- remove the cannula
- notify the medical team or senior nurse as further intervention may be required depending on the factors related to the injury13.
Elevation of the affected limb for up to 48 hours may help with reabsorption of the infiltrate. Local thermal treatment depends on the pharmacological agent infused and expert advice should be sought as to whether heat or cold is appropriate20.
If an extravasation injury does occur, ensure that the appropriate documentation is completed using an approved extravasation scale and following local policy for reporting13.
Correct PIVC placement and observation
Key factors to a successful infusion include ensuring correct placement and stabilisation of the cannula (with the patient reporting no pain or burning), and no swelling around the insertion site. The recommended guides should be carefully adhered to during infusion of any medication or fluid to reduce the risk of tissue injury and loss of the PIVC. The cannula insertion site should also be assessed and observed at least every four hours20.
Placement of PIVCs is recommended in forearm veins as opposed to the hand, wrist or ante-cubital fossa as the forearm sites are less prone to occlusion, accidental dislodgment and phlebitis21. Nurses are well placed to advocate for their patient to have a central venous access device (CVAD) placed for the administration of vesicant medications18.
Flushing protocols and administration of IV medications
There is very little research and a high degree of practice variation in the maintenance of PIVC, including the role of flushing to prevent complications. It is highly recommended that nurses refer to the manufacturer’s guidelines and local organisational policy for the recommended preparation and speed of infusion in order to prevent vein injury21. For example: 1.2g Amoxicillin plus Clavulanic Acid (Augmentin). Administration notes: Inject slowly over three to four minutes22.
Good documentation
Documentation is essential for accountability, as well as the maintenance of a high standard of professional practice; however, it is often overlooked, especially when the workload is high21.
The use of a pre-printed care plan can be useful. An example used in one New Zealand hospital includes documentation of:
- Patient information and consent
- date and time of insertion
- name and signature of cannulator
- location, type and gauge of cannula
- indication for use.
- Ongoing care documentation should include:
- cannula checked & cannula required
- needleless access device insitu
- dressing intact & dated
- cannula flushed (flush solution)
- VIP score & indication for use
- cannula removed – including date, time and reason12,13,21.
Conclusion
Early recognition of IV complications through regular assessment and observation enables appropriate and timely intervention, minimising disruption to the patient’s treatment, improving patient outcomes, as well as reducing healthcare costs involved in extra treatment and procedural requirements and increased bed days from unnecessary complications.
The following quote reinforces the intent of this article:
“Penetration of a patient’s natural protective skin barrier with a foreign body that directly connects the outside world to the bloodstream for a prolonged period of time is not to be taken lightly. Insertion of an IV catheter is an invasive procedure that introduces multiple risks and potential morbidities, and even mortalities, and should be given the respect that it deserves.”23
View PDF of this article (and related learning activity) here >>
Recommended Resources
AVATAR is an Australian-based teaching and research group aimed at “making vascular access complications history”: http://www.avatargroup.org.au
Intravenous Nursing New Zealand (IVNNZ Inc.) is a voluntary, non-profit, professional development organisation and affiliated international member of the Infusion Nurses Society (INS) and is dedicated to Best Practice Recommendations and Standards of Practice for Infusion Therapy: http://www.ivnnz.co.nz/
Infusion Nurses Society (2016.) Infusion Therapy Standards of Practice Journal of Infusion Nursing. 39 (1S)
About the author:
Bev Hopper MHPrac (Nursing), PG Cert Advanced Nursing Practice (Orthopaedics), BHSc (Nursing), NZRN (Comp) is the Clinical Nurse Specialist (Out Patient IV Antibiotics) at Waitemata District Health Board in Auckland.
This article was peer reviewed by:
Catharine O’Hara RN MN is Clinical Nurse Specialist (Lead) Intravenous & Related Therapy at MidCentral District Health Board’s Department of Anaesthesia & ICU
Rachael Haldane, RN BN PGDip HSc is a clinical nurse specialist, infusion services for Nurse Maude, Christchurch.
REFERENCES
- Personal anecdote of Beverley Hopper.
- AHLQVIST M, BERGLUND B, NORDSTROM G, KLANG B ET AL. (2010).
A new reliable tool (PVC assess) for assessment of peripheral venous catheters. Journal of Evaluation in Clinical Practice 16 (6), 1108-15. - NURSING COUNCIL OF NEW ZEALAND (2007). Competencies for Registered Nurses. Retrieved September 2016 from www.nursingcouncil.org.nz/Publications/Standards-and-guidelines-for-nurses.
- OLIVEIRA A & PARREIRA P (2010). Nursing interventions and peripheral venous catheter-related phlebitis. Systematic literature review. Referência: Scientific Journal of the Health Sciences Research Unit: Nursing 3(2), 137-47.
- DOUGHERTY L (2008). Peripheral Cannulation. Nursing Standard 22 (52), 49-56.
- HIGGINSON R (2011). Phlebitis: treatment, care and prevention. Nursing Times 107 (36), 18-21.
- KOKOTIS K (2015). Preventing chemical phlebitis. Nursing 28 (11), 41-7.
- MACKLIN D (2003).Phlebitis: A painful complication of peripheral IV catheterization that may be prevented. The American Journal of Nursing 103(2), 55-60.
- HIGGINSON R (2015). IV cannula securement: protecting the patient from infection British Journal of Nursing (8)24, S23-S28.
- MALACH T, JERASSY Z, RUDENSKY B, SCHESINGER Y ET AL. (2006). Prospective surveillance of phlebitis associated with peripheral intravenous catheters. American Journal of Infection Control 34 (5), 308-12.
- RYDER M (2005). Catheter related infections: It’s all about the bio-film. Topics in Advanced Practice Nursing eJournal 5 (3).
- INFUSION THERAPY STANDARDS OF PRACTICE (2016). Retrieved September 2016 from www.anzctr.org.au/AnzctrAttachments/369954-INSper cent20Standardspercent20ofper cent20Practice 2016.pdf
- INTRAVENOUS NURSING NEW ZEALAND. (2012). Retrieved September 2016 www.ivnnz.co.nz/files/file/7672/IVNNZ_Inc_Provisional_Infusion_Therapy_Standards_of_Practice_March_2012.pdf.
- RAY-BARRUEL G, POLIT D, MURFIELD J & RICKARD C (2014). Infusion phlebitis assessment measures: a systematic review. Journal of Evaluation in Clinical Practice 20 (2), 191-202.
- WALLIS M, MCGRAIL M, WEBSTER J, MARSH N et al (2014). Risk factors for peripheral intravenous catheter failure: a multivariate analysis of data from a randomised control trial. Infection Control and Hospital Epidemiology 35 (1), 63-8.
- DA SILVA G, PRIEBE S, DIAS F (2010). Benefits of establishing an intravenous team and the standardisation of peripheral intravenous catheters. Journal of Infusion Nursing 33 (3), 156-60.
- WEBSTER J, MCGRAIL M, MARSH N, WALLIS M ET AL (2015). Post-infusion phlebitis: incidence and risk factors. Nursing Research and Practice, 2015.
- SIMONOV M, PITTIRUTI M, RICKARD C, CHOPRA V (2015). Navigating venous access: A guide for hospitalists. Journal of Hospital Medicine 10 (7), 471-8.
- SALGUIRO-OLIVEIRA A, PARREIRA P, VEIGA P (2012). Incidence of phlebitis in patients with peripheral intravenous catheters: the influence of some risk factors. Australian Journal of Advanced Nursing 30 (2), 32-9.
- DOELLMAN D, HADAWAY L, BOWE-GEDDES L A, FRANKLIN M, ET AL. (2009). Infiltration and extravasation: Update on prevention and management. Journal of Infusion Nursing 32 (4), 203-11.
- BROOKS N (2016). Intravenous cannula site management. Nursing Standard 30, 53-62.
- New Zealand Hospital Pharmacists Association (2015). Notes on injectable drugs (7th ed.) Wellington, New Zealand.
- HELM R, KLAUSNER J, KLEMPERER J, FLINT L, ET AL (2015). Accepted but unacceptable: Peripheral IV catheter failure. Journal of Infusion Nursing 38 (3), 189-203.
This learning activity is relevant to the Nursing Council competencies 1.1, 1.4, 2.1, 2.8, 2.9, 4.1, 4.2 and 4.3.
Learning outcomes
- define catheter-associated urinary tract infection (CAUTI)
- describe the pathogenesis of CAUTI
- identify risk-factors associated with CAUTI
- identify CAUTI prevention strategies that nurses can implement to promote patient safety.
 Introduction
Introduction
Catheter-associated urinary tract infection (CAUTI) is the most common healthcare-associated infection (HAI) worldwide1. Urinary tract infections (UTI) comprise 40 per cent of HAIs and 80 per cent of these UTIs are attributed to indwelling catheters2. Catheter-associated urinary tract infection complications include genito-urinary tract infections and life-threatening bloodstream infections that develop secondary to a UTI4.
The primary risk factor for CAUTI is the prolonged use of urinary catheters5. With the catheter in place, the daily risk for bacterial growth in the urine or bacteriuria is about 3 to 7 per cent6,7. Ten per cent of patients with bacteriuria will develop CAUTI, while three per cent will go on to develop bloodstream infections. Bloodstream infections result in discomfort, prolonged hospital stays, increased costs and, sometimes, deaths3,4,8.
CAUTI events are costly for both the patient and the entire healthcare system7,9. The clinical consequences and economic burden of CAUTI makes CAUTI prevention fundamental to patient safety. (See Box 1 below for definition of CAUTI)
CAUTI pathogenesis
Indwelling urinary catheters are used therapeutically to drain urine from the bladder; however, when used inappropriately, catheters can pose both mechanical and physiological risks to patients1.
Catheters cause mechanical erosion of the bladder mucosa and ischemic damage when swelling occurs due to blockage. Catheters also provide a route for microbial entry from the colonised perineum to the sterile bladder through a catheter’s internal and external surfaces1. Microorganisms that colonise the perineum and intestinal tract cause about two-thirds of CAUTI, while a third are caused by urine collection systems contaminated by healthcare workers’ hands11.
Urinary catheters interrupt the normal bladder defence mechanism1,11. When bacteria are present in the urinary system, the bacteria bind to the sterile mucosa, which starts an inflammatory response characterised by the inflow of neutrophils and shedding of epithelial cells12. When the catheter is in place, the bacteria bind to catheter surfaces and form a biofilm, which bypasses the normal bladder defence mechanism11.
Biofilm
Biofilm formation is central in the development of CAUTI12. Biofilms are slimy structures made up of communities of microorganisms. Biofilm forms when a conditioning film of host components attaches itself to the inner and outer surface of a urinary catheter after insertion. Biofilm traps free-swimming microorganisms that then multiply, attract more microorganisms, and further secrete extracellular matrix that makes the biofilm grow in size. Biofilm microorganisms function as a community and communicate closely with one another1,13. Some microorganisms also detach from the biofilm and seed the urine1.
Biofilms help microorganisms survive through: resistance to being swept away by shear forces; resistance to being engulfed by other cells, and resistance to antimicrobial agents1,13. Studies have shown that antimicrobial agents penetrate biofilms; however, the slow growth of microorganisms in a biofilm confers antimicrobial resistance11. The affinity of microorganisms with each other in a biofilm also permits the exchange of antimicrobial resistance genes, thereby increasing the risk for other CAUTI complications12.
Risk factors for CAUTI
Prolonged catheterisation is the major risk factor for CAUTI3,5. Other risk factors include: non-adherence to aseptic technique during catheter insertion11; poor hand hygiene compliance8; catheter insertion after the sixth day of hospitalisation; poor hand hygiene; catheter insertion outside the operating room9, and a break in the closed drainage system8,14.
Strategies to prevent CAUTI
Multiple strategies have been shown to prevent CAUTI. Prevention strategies were published by the US CDC in 1981 and subsequently updated in 20098 and 20143. These strategies and recommendations were summarised by the USA-based Institute for Healthcare Improvement (IHI)7 into four components of urinary catheter care. Australia and New Zealand’s 2013 catheterisation guidelines break down the principles for reducing CAUTI into similar sections or components, but with the addition of a section on selecting the appropriate catheter type and drainage system18. The following discussion expands on those components of care to include other evidence-based recommendations.
Component One: Reduce inappropriate use of urinary catheters
Urinary catheter presence in the bladder is the primary risk for CAUTI; thus, reducing inappropriate use is the best way to prevent it11,15.
Catheters should only be inserted when clinically indicated.
Some indications for using short-term catheterisation are:
- acute and chronic urinary retention
- urinary obstruction
- close monitoring of fluid intake and output of critically ill patients
- risk of worsening sacral decubitus ulcer due to urinary incontinence or end-of life care5,8,16,17
- selected surgical procedures that last more than three hours
- management of acute urologic conditions when straight catheterisation is not possible8,16,17
- patients undergoing urologic surgery or surgery on other genitourinary tract structures
- patients anticipated to receive large-volume infusions or diuretics during surgery, and the need for intraoperative monitoring of urinary output.
- urinary catheterisation may also be indicated for patients requiring prolonged immobilisation8.
Inappropriate indications for using indwelling catheters include:
- as a substitute for nursing care of incontinent patients
- as a means of obtaining urine for culture when the patient can voluntarily void8
- for prolonged postoperative duration without appropriate indications8.
Nurses are also encouraged to: use a bladder scanner in assessing urine volume to reduce unnecessary catheter insertions, and consider other bladder management methods such as intermittent catheterisation3,8.
Component Two: Perform proper techniques for indwelling catheter insertion
Indwelling catheter insertion is an invasive procedure that requires care and proper technique to avoid pain, trauma and infection. For more guidance you can view the best-practice urinary catheterisation guidelines [see recommended resources] developed by the Australia and New Zealand Urological Nurses Society (ANZUNS)18.
Selection of catheter
- Select appropriate length and type of catheter for patient.
- Use smallest gauge catheter possible, while ensuring good drainage to minimise bladder neck and urethral trauma3,8.
Hand hygiene
Hand hygiene before and after catheter insertion prevents the introduction of microorganisms into the catheter, thereby minimising CAUTI risk3,8.
Aseptic technique and the use of sterile equipment
Aseptic technique minimises the risk of microbial entry into the sterile urinary system. Aseptic technique during catheter insertion, the use of sterile equipment, and even the setting of catheter insertion all play a significant role in reducing the incidence of bacteriuria19. The use of sterile gloves, drape, sponges, an appropriate antiseptic or sterile solution for periurethral cleaning, and a single-use packet of lubricant jelly for insertion is recommended8.
Secure indwelling catheters after insertion to prevent movement and urethral traction
Indwelling catheters should be kept secure to minimise movement that may cause urethral trauma or erosion of the bladder mucosa7,8,20. Trauma to the bladder mucosa releases organic molecules, which, when combined with glycoprotein from the urine, facilitate bacterial colonisation, thereby increasing CAUTI risk12.
Component Three: Implement proper urinary catheter maintenance procedures
Proper maintenance of urinary catheters focuses on maintaining a closed system and maintaining an unobstructed urine flow8. Ongoing good hand and general hygiene is also very important3,8.
Maintain a closed drainage system
Urinary drainage systems should remain closed because disconnections at the catheter-collecting tube junctions have been shown to significantly increase bacteriuria risk due to bacterial spread along the internal surface of the catheter.
The relative risk of acquiring CAUTI the day after catheter disconnection has been shown to double21. If there are breaks in aseptic technique, disconnection or leakage, nurses should replace the catheter and collection bag using aseptic technique and sterile equipment8.
Microbial spread along the internal catheter surface can also happen if urine in the collection bag is contaminated through improper emptying. In this way microorganisms can gain access to the drainage system and ascend to the bladder, particularly if standard precautions are not observed22. When draining the bag, nurses are also encouraged to avoid splashing urine, to use a separate clean collecting container for each patient, and to prevent contact of the drainage spigot with the non-sterile collecting container3,8,20.
The CDC further recommends that the collection of urine samples should be performed aseptically through the needleless sampling port or the drainage bag using a sterile syringe/cannula after the port is cleansed with a disinfectant8.
Maintain an unobstructed urine flow
Unobstructed urine flow can be achieved through the following measures: keeping the catheter and collection bag free from coils or kinks and off the floor at all times, and emptying the collection bag regularly3,8,20,23.
A study conducted among intensive care patients showed that drainage tubing kinking or coiling was significantly associated with fever and bacteria in the urine23. The presence of kinks and coils is thought to compromise bladder emptying and possibly increase bladder hydrostatic pressure, thereby causing transient bacteriuria, thus the fevers.
The recommendation that the collection tubing and bag should always remain below the patient’s bladder to allow proper urine drainage is supported by a large prospective study in the US showing that improper positioning of the collection tubing and bag is associated with a significantly increased risk in CAUTI because of the backflow of potentially contaminated urine from the drainage bag24.
The authors of a European microbiology study explain that when the drainage bag is placed above the level of the bladder, microorganisms from the urine bag can gain access to the drainage system along the internal catheter surface and ascend to the bladder22.
Component Four: Review catheter necessity daily and remove promptly
The length of time a urinary catheter is in place is the strongest predictor of CAUTI development8. Recommendations indicate that indwelling urinary catheters should be removed as soon as possible post-operatively, preferably within 24 hours unless there are indications for continued use8. It has been found that patients develop bacteriuria at a rate of three to seven per cent per day7. This risk increases to 25 per cent when the catheter remains in place for one week and increases to nearly 100 per cent when the catheter remains in place for up to a month7.
Effective catheter care involves collaborative effort8; however, nurses remain largely responsible for indwelling catheter care. Daily assessment of catheter need and the possibility of removal is recommended3, with electronic alerts or other daily reminder systems important in acute care. Nurses are also advised to use standard precautions during catheter removal to prevent cross-transmission of microorganisms, thereby preventing CAUTI8.
Conclusion
In summary, the components of care to prevent CAUTI include: reduction of inappropriate use of urinary catheters; performance of proper indwelling catheter insertion techniques; selection of correct catheter and drainage system; implementation of proper catheter maintenance procedures, and removal of catheters in a timely manner.
These catheter management components are all inter-related and can help to prevent this most common of the healthcare-associated infections – CAUTI.
In addition, education on CAUTI prevention should not only focus on one aspect of care, but should also be spread across all components
of care.
Box 1: CAUTI definition
The definition of CAUTI varies worldwide, as does the criteria for identifying CAUTI. One of the more commonly used definitions in acute care settings is that of the National Healthcare Safety Network (NHSN) of the United States Government’s Centers for Disease Control and Prevention (CDC). The NHSN define CAUTI as a urinary tract infection in a person with an indwelling urinary catheter for more than two days and at least one of the following criteria:
- With catheter still in place, the person develops at least one of the following – fever (> 38C), suprapubic tenderness, costovertebral angle pain, and a positive urine culture of > 105 colony-forming units (CFU)/ml with no more than two species of microorganisms.
- With catheter removed the day prior to, or on the day, the person manifests at least one of the following – fever (> 38C), urgency, frequency, dysuria, suprapubic tenderness, costovertebral angle pain, and a positive urine culture of > 105 CFU/ml with no more than two species of microorganisms (reference 10).
View the PDF of this article (and related learning activity) here >>
Recommended resources:
Detailed best-practice urinary catheterisation guidelines from the Australia and New Zealand Urological nurses Society (ANZUNS) can be downloaded from their website at www.anzuns.org
Evidence-based guidance on the prevention of healthcare-associated infections in primary and community care can be found at the National Institute for Health and Care Excellence (NICE) website at www.nice.org.uk/guidance/cg139/evidence
The CDC website also offers resources for both patients and healthcare workers. The CDC guideline for CAUTI prevention is downloadable from their website at https://www.cdc.gov/infectioncontrol/guidelines/cauti/index.html
About the authors:
- Monina Gesmundo RN, BSN, PGCertTT, PGDipHSc, MNur (Hons) until recently worked as a clinical nurse specialist for infection prevention and control at Counties Manukau Health. She is currently a lecturer at the School of Nursing, Massey University.
- Dr Anna King is a lecturer at the School of Nursing, the University of Auckland.
Lisa Stewart, RN, BA, PGDipHSc, MNur (Hons) is a professional teaching fellow and PhD candidate at the School of Nursing, the University of Auckland.
This article was peer reviewed by:
- Ruth Barratt RN BSc MAdvPrac (Hons), a clinical nurse specialist infection prevention and control for the Canterbury District Health Board.
REFERENCES
- SIDDIQ D & DAROUICHE R (2012). New strategies to prevent catheter-urinary tract infections. Nature Reviews Urology, 9, 305-314.
- WEBER D, SICKBERT-BENNETT E, GOULD C ET AL. (2011). Incidence of catheter-associated and non-catheter-associated urinary tract infections in a healthcare system. Infection Control & Hospital Epidemiology, 32(8), 822-823.
http://dx.doi.org/10.1086/661107 - LO E, NICOLLE L, COFFIN S ET AL. (2014). Strategies to prevent catheter- associated urinary tract infections in acute care hospitals: 2014 update. Infection Control and Hospital Epidemiology, 35(5), 464-479. doi:10.1086/675718
- CENTERS FOR DISEASE CONTROL (2013). April 2013 CDC/NHSN protocol corrections,clarification, and additions. Retrieved from
https://www.cdc.gov/nhsn/pdfs/pscmanual/7psccauticurrent.pdf - MOHAJER M & DAROUICHE R (2013). Prevention and treatment of urinary catheter-associated infections. Current Infectious Disease Reports, 15(2), 116-123.
- REBMANN T & GREENE L (2010). Preventing catheter-associated urinary tract infections: An executive summary of the Association for Professionals in Infection Control and Epidemiology, Inc, elimination guide. American Journal of Infection Control, 38(8), 644-646.
- INSTITUTE FOR HEALTHCARE IMPROVEMENT (2011). How to guide: Prevent catheter-associated urinary tract infection. Retrieved from http://www.ihi.org/Topics/CAUTI/Pages/default.aspx
- GOULD C., UMSCHEID C, AGARWAL R, ET AL. (2009). Guideline for prevention of catheter-associated urinary tract infections. Retrieved from
www.cdc.gov/hicpac/pdf/cauti/cautiguideline2009final.pdf - BURTON D, EDWARDS J, SRINIVASAN A ET AL. (2011). Trends in catheter-associated urinary tract infections in adult intensive care units – United States, 1990–2007. Infection Control and Hospital Epidemiology, 32(8), 748-756
- CENTERS FOR DISEASE CONTROL (2015). Urinary tract infection (catheter-associated urinary tract infection and non-catheter-associated urinary tract infection and other urinary system infection events. Retrieved from
www.cdc.gov/nhsn/PDFs/pscManual/7pscCAUTIcurrent.pdf - CHENOWETH C & SAINT S (2013). Preventing catheter-associated urinary tract infections in the intensive care unit. Critical Care Clinics, 29(1), 19-32 doi:10.1016/j.ccc.2012.10.005
- TRAUTNER B & DAROUICHE R (2004). Role of biofilm in catheter-associated urinary tract infection. American Journal of Infection Control, 32, 177-183.
- NIKOLAEV Y, & PLAKUNOV A (2007). Biofilm -“City of microbes” or an analogue of multicellular organisms? Microbiology, 76(2), 125-138.
- KING C, GARCIA ALVAREZ L, HOLMES A ET AL. (2012). Risk factors for healthcare-associated urinary tract infection and their applications in surveillance using hospital administrative data: a systematic review. Journal of Hospital Infection, 82, 219-226.
- BERNARD M, HUNTER K & MOORE K (2012). A review of strategies to decrease the duration of indwelling urethral catheters and potentially reduce the incidence of catheter-associated urinary tract infections. Urologic Nursing, 32(1), 29-37.
- TITSWORTH W, HESTER J, CORREIA T ET AL. (2012). Reduction of catheter-associated urinary tract infections among patients in a neurological intensive care unit: A single institution’s success. Journal of Neurosurgery, 116(4), 911-920.
http://dx.doi.org/10.3171/2011.11.JNS11974 - MURPHY C, FADER M & PRIETO J (2013). Interventions to minimise the initial use of indwelling urinary catheters in acute care: a systematic review. International Journal of Nursing Studies, 1-10.
- AUSTRALIA AND NEW ZEALAND UROLOGICAL NURSES SOCIETY CATHETERISATION GUIDELINE WORKING PARTY (2013). Catheterisation Clinical Guidelines. ANZUNS, Victoria.
www.anzuns.org/wp-content/uploads/2015/03/ANZUNS-Guidelines_Catheterisation-Clinical-Guidelines.pdf - BARBADORO P, LABRICCIOSA F, RECANATINI C, ET AL. (2015). Catheter-associated urinary tract infection: Role of the setting of catheter insertion. American Journal of Infection Control, 43(7), 707-710.
- HOOTON T, BRADLEY S, CARDENAS D ET AL. (2010). Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 international clinical practice guidelines from the Infectious Diseases Society of America. Clinical Infectious Diseases, 50(5),625-663. doi:10.1086/650482
- PLATT R, MURDOCK B, FRANK POLK B, & ROSNER B (1983). Reduction of mortality associated with nosocomial urinary tract infection. The Lancet, 321(8330), 893-897. doi:10.1016/S0140-6736(83)91327-2
- WENZLER-RÖTTELE, DETTENKOFER, SCHMIDT-EISENLOHR ET AL. (2006). Comparison in a laboratory model between the performance of a urinary closed system bag with double non-return valve and that of a single valve system. Infection, 34(4), 214-218.
- KUBILAY Z, LAYON A, KUBILAY Z ET AL. (2013). What we don’t know may hurt us: Urinary drainage system tubing coils and CAUTIs – A prospective quality study. American Journal of Infection Control, 41(12),1278-1280. doi:10.1016/j.ajic.2013.06.009
- MAKI D, & TAMBYAH P (2001). Engineering out the risk for infection with urinary catheters. Emerging Infectious Diseases, 7(2), 342.
This learning activity is relevant to the Nursing Council competencies 1.4, 1.5, 2.1, 2.8, 3.1, 3.2 & 3.3.
Learning outcomes
- increase your knowledge of novel psychoactive substances (NPS) and how they affect mental health
- identify potential physical health and mental health risks resulting from NPS use for clients in your area of nursing
- increase your understanding of co-existing substance use and mental health problems and some approaches to managing clients that misuse substances like NPS.
Introduction
Novel psychoactive substances (NPS) or the so-called ‘legal highs’ are emerging rapidly worldwide, as are concerns about NPS abuse.
NPS have been a growing trend over the past decade for a number of reasons, including difficulties detecting them in routine urine drug screens, legal loopholes, easy access through the internet and low cost1.
Labelling these drugs as ‘herbal highs’ or ‘legal highs’ is misleading as there is nothing natural about these synthetic and untested drugs and also currently none of them are legal in New Zealand2. But there has been an explosion in numbers of NPS worldwide with the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) reporting this year that it is now monitoring 560 NPS and 98 new substances that were reported for the first in 2015 and 101 in 20143.
There are several typical categories of NPS drugs including synthetic cathinones (e.g. mephedrone and MDPV), plant-based NPS (e.g. khat and salvia divinorum), synthetic cannabinoids (e.g ‘Spice’, ‘Kronic’ and ‘K2’), and ‘party’ drugs like benzylpiperazine (BZP).
Synthetic drugs can be taken through insufflation (snorting), oral ingestion and rectal insertion, as well as being taken intravenously, intramuscularly and subcutaneously.
These drugs are considered to have an effect on mental health wellbeing. Identified mental health symptoms that can result from NPS use are low mood, confusion, and anxiety1.
The European Monitoring Centre for Drugs and Drug Addiction (EMCDDA)4 identified synthetic cannabinoids as prominent in affecting mood and perception and that intoxications can cause agitation, tachycardia, and arterial hypertension. The centre says that synthetic cannabinoids are 100 times more powerful than traditional strains of cannabis4.
The EMCDDA also identified synthetic cathinones as hallucinogenic stimulants with cardiovascular and psychiatric side effects.
The number of deaths involving NPS increased by 15 per cent in 2013 in the United Kingdom, with 60 deaths, up from 52 deaths in 20125. New Zealand attempted temporary bans on different NPS before passing the Psychoactive Substances Act in 2013, which puts the responsibility on NPS producers or importers to prove they are low risk6. At present no NPS products are legally available for sale in New Zealand2, but the the ingredients for making illicit drugs are still available for purchase on untraceable internet sites so access to NPS continues.
Detection of NPS use can be difficult as adult users – who usually present with agitation, cardiovascular and psychiatric symptoms – can often pass urine drug screening due to the lack of detectable metabolites. To further complicate matters, the molecular makeup of NPS drugs can be changed slightly to make detection through urine drug screening tests even more difficult7.
It has been suggested that health professionals, for example, in emergency departments, primary health and mental health services, need to be made aware of the growing levels of NPS misuse so that it can be identified and treated accordingly7.
Examples of NPS and the risks they could pose to the people you nurse
It is useful for nurses to have an understanding of the potential risks of NPS. Nurses also need to maintain a therapeutic relationship that is respectful of the individual’s choices, experiences and expertise11,12.
This section looks at some of the NPS currently available.
Synthetic cathinones
Mephedrone is one of a group of synthetic cathinone drugs that are chemically similar to amphetamines. Another is methylenedioxypyrovalerone (MDPV). Synthetic cathinones can result in the stimulation of psychosis, neurological and other health complications. Mental health professional intervention is needed for people with mental health problems as a result of mephedrone misuse.
Synthetic cathinones have been found to have similar effects to psychostimulatory drugs of misuse including cocaine, amphetamine and MDMA (ecstasy). Psychiatric symptoms as a result of mephedrone/cathinone misuse include aggression, agitation, anhedonia, anxiety, confusion, delusions, depression, dysphoria, irritability, loosening of association, mental fatigue, panic attacks, paranoia, perceptual distortion, psychosis, self-mutilation, suicidal thoughts/suicide and visual and auditory hallucinations. Addictive symptoms identified include tolerance, craving and withdrawal syndrome13.
’N-Bomb’ or NBOMe
The psychedelic drug commonly known as ‘N-Bomb’ (25I-NBOMe, 2C-I-NBOMe) is a powerful hallucinogen that has been prevalent in New Zealand since 201214. N-Bomb’s high potency increases risks of toxicity in small doses. Common routes of administration include sublingual, buccal, and nasal/intranasal15.
The hallucinogenic effects of N-Bombs mimic LSD and can last between six and 10 hours and include feelings of euphoria, mental and physical stimulation, a pleasant or positive change in consciousness and unusual body sensations. Risks include tachycardia, hypertension, pyrexia, agitation, hallucinations, seizures and death. There have been media reports in New Zealand of renal and cardiovascular complications following use and overseas there have been a number of N-Bomb-related deaths14.
Spice and other synthetic cannabinoids
The misuse of ‘Spice’ or synthetic cannabinoids is increasing among teenagers and adults. Spice has over 220 compounds in various different combinations or brands16. There is also a risk of Spice causing psychopathological disturbances, namely psychosis, causing what is known as “Spiceophrenia”.
Spice can affect a person’s physical state and can trigger vomiting, seizures, tachycardia, mydriasis, hypertension, confusion and restlessness. Mental health symptoms include delusions, paranoia, disorganised thought and visual and auditory hallucinations. Fluctuating mood, anxiety, perception, thinking, memory, and attention is common. Agitation, panic, dysphoria, psychosis and bizarre behaviour are also common17.
Khat*
The khat plant, better known as ‘Catha edulis’, has been chewed by Eastern Somalian and some Islamic communities since 640 AD. Over the past century synthetic cathinones have been derived from this traditional plant to produce NPS.
Khat is known for its stimulant effect similar to amphetamine; there have been numerous disputes around the mental health harms of using khat27, but there is an increased risk for psychotic episodes, similar to stimulant (cocaine or amphetamine) and drug-induced psychosis28.
GHB and GBL*
GHB (gamma-hydroxybutyrate) and GBL (gamma-butyrolactone) are illicit drugs with similar sedative and anaesthetic effects. GBL is converted to GHB shortly after entering the body. Both produce a feeling of euphoria and can reduce inhibitions and cause sleepiness. Dependence is rare but users of these compounds can develop tolerance and cravings. Many users complain of insomnia, anxiety and depression29
Ketamine and 3-MeO-PCP*
Other illicit drugs that affect mental health include ketamine, which is a short-acting dissociate (a class of hallucinogens) compound with anaesthetic and analgesic use. Ketamine’s effects reportedly last two hours and visual hallucinations are common.
Transient psychological experiences include anxiety, paranoia and disturbing hallucinations20. Another dissociative anaesthetic drug marketed as an NPS is 3-Methoxyphencyclidine (3-MeO-PCP). There is also some clinical evidence to suggest that intravenous ketamine infusion has been found to be safe and effective for refractory depression and suicidal ideation. However, this is not practical for maintenance therapy long term30.
Why may people who experience MH issues use NPS?
There are various reasons for the prevalence of people with mental health problems abusing illicit substances like NPS. This includes the cheap availability of NPS, accessibility and peer pressure1.
Also, according to Ponizovsky et al18, people with co-existing problems are more at risk of non-adherence to prescribed medication and therefore more prone to relapse, rehospitalisation, and illicit drug and alcohol use.
One recent research study talks about mental health service users using illicit drugs to control their distressing symptoms, or to “relax” and to get “high”19. The findings of this empirical study suggest that substance use was related to controlling emotional states, anxiety, and depression. Alcohol was seen as less harmful than cannabis and other psychoactive compounds in the perception of the mentally ill substance user. Counteracting psychiatric medication side effects was also identified as a reason, alongside controlling psychotic states, i.e. managing auditory hallucinations by smoking more cannabis. So nurses should be aware that some clients may ‘manage’ mental health symptoms with illicit drugs and alcohol.
Mental health professionals use a range of patient-centred and focused risk assessments that have been formulated specifically for people with co-existing problems9,20.
One harm reduction approach to tackling NPS or other substance misuse, that can be done in non-specialist addiction settings like primary health, is using a brief assessment tool to assess whether alcohol or drug problems are at the ‘social or harmless use’ end of the continuum or the ‘moderate to severe’. This helps identify the level of intervention needed with mild problems usually just needing a brief intervention to reduce use to safe levels, while ‘moderate to severe’ problems require a comprehensive assessment and management plan9.
Co-existing problem approaches
The New Zealand guidelines for the assessment and management of co-existing problems9 take a client-centred approach.
The guidelines set out seven key principles, including screening all clients presenting in mental health and addiction services for CEP and, if positive, undertaking a comprehensive assessment that gives equal weight to both mental health and substance use problems. Also emphasised is safety, stabilisation, engaging with clients by developing a ‘trusting, empathetic and non-judgemental therapeutic relationship’, taking cultural needs and general wellbeing into consideration; and that CEP management should include strategies to enhance motivation, deliver interventions appropriate to the nature and severity of the problems, and provide integrated care9.
Barriers to CEP treatment can be prevalent across health settings due to miscommunication, lack of awareness and inappropriate referrals between mental health, substance misuse and community services8. There is a need for co-ordination between services, effective policies, protocols and effective clinical leadership. A clear referral pathway to addiction and mental health services is also needed8.
Psychosocial interventions helpful for clients who use NPS
Psychosocial interventions can be beneficial in the treatment of substance use problems including NPS.
The traditional approach for treating drug problems includes medication approaches and psychosocial (psychology-based) interventions. Psychosocial interventions include treatments such as cognitive behavioural therapy (CBT) that aims to modify cognitive processes and behaviour21 and can be used as an approach to enhance subjective wellbeing8.
Motivational interviewing (MI) is a common psychosocial intervention aimed at enhancing motivation and readiness for treatment. Miller and Rollnick define motivational interviewing as a non-judgmental, non-confrontational and non-adversarial approach that enhances a person’s awareness of the problems caused and the consequences experienced as a result of their behaviour e.g. alcohol dependence22.
Motivation – including strategies to enhance motivation like CEP-adapted motivational interviewing (MI) – is one of the seven key principles of CEP treatment in New Zealand9. New developments in MI include an increased emphasis on the client’s hopes and values and structured first interviews aimed at enhancing engagement in treatment9.
Contingency management is another psychosocial technique that provides a system of incentives or reinforcement to encourage abstinence. Dutra et al23 suggest drug abstinence increased by using strategies such as food vouchers, money or other incentives for positive behaviour. Other emerging psychosocial approaches that the 2010 New Zealand guidelines say show promise include kaupapa Māori approaches, mindfulness, and acceptance and commitment therapy9.
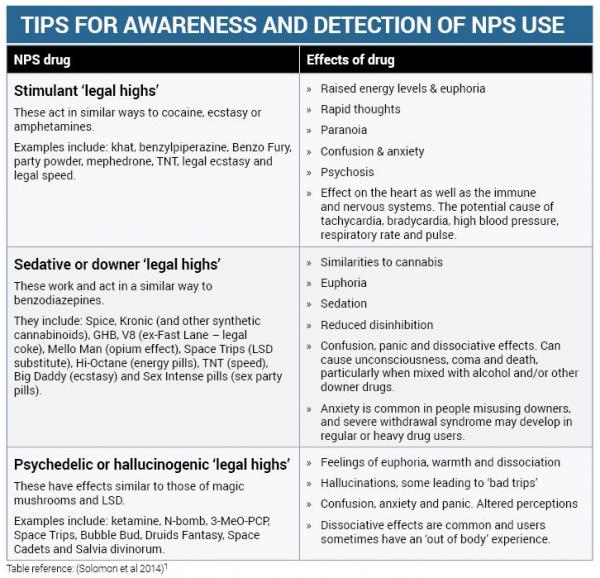
Co-existing problems
Mental health problems are widely associated with substance misuse, including the use of legal highs. There are a range of terms used to describe this combination of problems, including dual diagnosis, but the term ‘co-existing substance use and mental health problems’, or co-existing problems (CEP) for short, is used in New Zealand with ‘co-existing’ chosen as it implies interaction more than ‘co-occurring’8.
CEP are highly prevalent in therapeutic settings in New Zealand with an estimated third to half of all tangata whaiora (service clients) in mental health settings likely to have current CEP and up to three-quarters of clients seeing addiction services9. People with severe CEP experience higher rates of institutionalisation, more failed treatment attempts, poverty, homelessness and risk of suicide8.
It is estimated that 40 per cent of people with psychosis also have substance misuse problems. People with co-existing substance use and mental health disorders have higher rates of unmet needs and a higher rate of relapse and hospitalisation than those who primarily have psychosis10.
It has been identified that some people with psychosis commonly misuse non-prescribed medication to deal with persisting psychiatric symptoms, which ultimately exacerbate psychiatric symptoms10.
Conclusion
Mental health problems as a result of adults misusing novel psychoactive substances (NPS) are emerging around the world and in New Zealand. Despite law changes, NPS – and the ingredients to make illicit drugs – are available to purchase on hidden internet sites that are untraceable to law enforcement worldwide.
There is a push in New Zealand to address co-existing problems (CEP) of mental health and substance use with strategies and guidelines8,9 and an updated blueprint for mental health24.
CEP is highly prevalent in New Zealand and NPS is a newly contributing factor. Therefore it is important that nurses have a knowledge and understanding of substance use and CEP issues in general, including the common effects and risks of NPS use.
Collaboration and partnerships between mental health, addiction, primary care and other areas of nursing are essential to providing a safe and harm reduction approach to substance misuse. Monitoring, early detection, engagement with clients and using suitable interventions are very important in minimising harm from NPS and other substance use. These approaches are inherent to the addiction nursing framework25, the mental health nursing standards of practice and the New Zealand College of Mental Health Nurses credentialing programme for primary care nurses26.
At present the research on managing NPS misuse is limited and there is a need to identify interventions that health professionals agree can work in managing co-existing problems resulting from NPS misuse. Services also need to respond early to communication problems and interface issues between services that can create barriers for CEP clients receiving access to mental health and drug treatments.
Poor mental health is disempowering for substance users and health professionals need to acknowledge personal experiences, empower recovery and improve the quality of life for people with mental health issues11,12.
View PDF of this article (including related learning activity) here >>
Recommended further resources
New Zealand Drug Foundation: Aimed at preventing and reducing harm from drug use and includes information on NPS used in New Zealand www.drugfoundation.org.nz
Psychoactive Substances Regulatory Authority: Information on New Zealand’s ‘legal highs’ regulation system
http://psychoactives.health.govt.nz
NEPTUNE (Novel Psychoactive Treatment UK Network): guidance on managing harm from NPS http://goo.gl/XZ4WN1
Toxinz: National poisons information database www.toxinz.com
NICE (National Institute for Health and Care Excellence): UK site with pathway for psychosis with coexisting substance misuse http://goo.gl/xC63LH
FRANK: UK site offering ‘friendly, confidential drugs advice’ www.talktofrank.com/drug/n-bomb
About the authors:
David Solomon MSc, PG Cert HE, BSc (Hons), Fellow of Higher Education. Independent Prescriber; RMN. Senior Lecturer, Nurse, Faculty of Health, Social Care and Education, Essex, Anglia Ruskin University.
Bernadette Solomon DHSc candidate, MSc (Applied Criminology), PG Cert HE, RMN. Professional Teaching Fellow, Faculty of Medical and Health Sciences: Mental Health and Addictions, the University of Auckland, New Zealand.
This article was peer reviewed by:
Daryle Deering RN PhD is a senior lecturer at the National Addiction Centre, the University of Otago.
Louise Leonard RN NP BA (Psych) MNurs is a nurse practitioner working in alcohol and other drug addictions for Waikato District Health Board’s mental health and addiction services.
*These sections were cut from the print version of the article and have been re-instated into the online version with references added to bottom of reference list.
REFERENCES
- Solomon D, Grewal P, Taylor C, Solomon B (2014). Managing misuse of novel psychoactive substances. Nursing Times 110(22): 12-15.
- Psychoactive Substances Regulatory Authority (2016) http://psychoactives.health.govt.nz (accessed June 20 2016).
- European Monitoring Centre for Drugs and Drug Addiction (2016) European Drug Report 2016: Trends and Developments. http://goo.gl/mZviw5
- European Monitoring Centre for Drugs and Drug Addiction (2013). European Drug Report 2013: Trends and Developments.
- Office for National Statistics (2013) Deaths related to drug poisoning in England and Wales: 2013. http://goo.gl/nq8wkg
- NZ Drug Foundation (2014) http://goo.gl/hNxNYV (accessed June 20 2016).
- Bajaj J, Mullen D, Wylie S (2010) Dependence and psychosis with 4-methylmethcathinone (mephedrone) use. BMJ Case Reports 2010.
- Ministry of Health (2010). Service delivery for people with co-existing mental health and addiction problems. Ministry of Health, Wellington.
- Todd F (2010) Te Ariari o te Oranga: The assessment and management of people with co-existing mental health and substance use problems. Ministry of Health, Wellington.
- Copello A, Walsh K et al (2013). A consultation-liaison service on integrated treatment: A program description Journal of Dual Diagnosis 9(2): 149-157.
- Barker P (2001). The Tidal Model: developing an empowering, person-centred approach to recovery within psychiatric and mental health nursing. Journal of Psychiatric and Mental Health Nursing 8: 233-240.
- Barker P, Buchanan P (2011). Myth of mental health nursing and the challenge of recovery. International Journal of Mental Health Nursing 20: 337-344.
- Advisory Council on the Misuse of Drugs (2010). ACMD report on the consideration of the cathinones. London. Available at www.homeoffice.gov.uk.
- NZ Drug Foundation (2014). http://drugfoundation.org.nz/matters-of-substance/NBOMe (accessed June 22 2016)
- Rose S, Poklis J, Poklis A (2013). A case of 25I-NBOMe (25-I) intoxication: a new potent 5-HT2A agonist designer drug. Clinical Toxicology 51: 174-177.
- Schifano F, Corazza O, Deluca P, Davey P, Davey Z (2009). Psychoactive drug or mystical incense? Overview of the online available information on Spice products. Journal of Culture and Mental Health 2(2): 137-144.
- Mustata C, Torrens M, Pardo R, Perez C et al (2009). The Psychonaut Web Mapping Group. Spice drugs: Cannabinoids as new designer drugs [Spanish]. Adicciones 21(3): 181-186.
- Ponizovsky A et al (2015). Trends in dual diagnosis of severe mental illness and substance use disorders, 1996-2010, Israel. Drug and Alcohol Dependence 148.
- Petterson H, Ruud H et al (2013). Empirical study: Walking the fine line: Self-reported reasons for substance use in persons with severe mental illness. Int J Qualitative Stud Health Well-being 8: 21968.
- Matua Raki (2012). Co-existing problems (CEP) service checklist http://goo.gl/MIiBHc.
- Conrod P, Stewart S (2005). A critical look at dual-focused cognitive-behavioral treatments for comorbid substance use and psychiatric disorders: Strengths, limitations, and future directions. Journal of Cognitive Psychotherapy 19(3): 261-284.
- Miller W, Rollnick S (2002). Motivational interviewing: Preparing people for change. Guilford Press, New York.
- Dutra L et al (2008). A meta-analytic review of psychosocial interventions for substance use disorders. American Journal of Psychiatry 165(2): 179-187.
- Mental Health Commission (2012). Improving mental health and wellbeing for all New Zealanders: A companion document to Blueprint II. Accessed at: https://goo.gl/4dGv80.
- Drug and Alcohol Nurses of Australasia (2012). Addiction specialty nursing competency framework for New Zealand, Matua Raki, Wellington. http://goo.gl/9MlxWG
- New Zealand College of Mental Health Nurses (2012). Standards of Practice for Mental Health Nursing in New Zealand Aotearoa 3rd Edition. Te Ao Māramatanga New Zealand College of Mental Health Nurses, Auckland. www.nzcmhn.org.nz.
- Hoffman R, Mustafa A (2013). Concurrent use of khat and tobacco is associated with verbal learning and delayed recall deficits. Addiction 108(10).
- Warfa N, Klein A, Bhui K, Leavey G, Craig T et al (2007). Khat use and mental illness: a critical review. Soc Sci Med 65: 309-318.
- Winstock A, Mitcheson L (2012). New recreational drugs and the primary care approach to patients who use them. BMJ 344(288).
- Andrade C (2015). Ketamine safety and tolerability in clinical trials for treatment-resistant depression. J Clin Psychiatry 76(3): 247-252.
This learning activity is relevant to the Nursing Council competencies 1.4, 1.5, 2.1, 2.8, 3.1, 3.2 & 3.3. Discuss all your answers with a peer/s.
Learning outcomes
- increase your understanding of the experiences of individuals with aphasia
- reflect on factors within the health care environment that may negatively impact on communication with those individuals
- describe a range of nursing strategies to enhance communication with individuals experiencing aphasia.
Introduction
Before Ed was admitted to an aged residential care facility, he ran his own small but successful business, making the most of his gregarious personality to develop a loyal customer base. Following a serious stroke, he was wheelchair dependent, with little spoken language and mild difficulty processing the speech of others. (See box p.17)
Ed was reluctant to interact with other residents. He felt uncomfortable not being able to join in their conversations and mostly stayed in his room. Ed and I shared some common interests, and, as a staff member, I would visit him to talk about these.
I chatted, Ed laughed, occasionally cried, and sometimes used gestures to express his emotions. He spoke a few words – though his vocabulary was mostly limited to the words ‘yes’ or ‘no’, which were occasionally used appropriately, and a range of expletives.
I hoped that Ed enjoyed my visits but I also worried about whether what felt like such a one-sided exchange just added to his frustrations. Was there anything I could do differently as a nurse to enable Ed to participate more in these conversations?1
Aphasia is “an impairment of language, affecting the production or comprehension of speech and the ability to read and write”2. Aphasia is commonly categorised as either being expressive (knows what they want to say, difficulty with speech and writing), receptive (difficulty with understanding spoken or written words), or global (few recognisable words, understands little or no spoken language)2. There can be considerable variation, however, in which and how many aspects of communication are impaired, and the severity of symptoms (see box p. 17) and it is vital that staff who are working with these individuals are aware of which aspects of language have been affected.
Aphasia does not mean there has been a loss of intelligence, although this is often assumed. While aphasia can result from traumatic brain injury or disease processes such as tumours, the major cause is stroke2. Each year approximately 9,000 New Zealanders experience a stroke, a quarter of whom will be under 65 years old3. Between 25 and 33 per cent of stroke survivors will have some degree of aphasia4,5, with only about 40 per cent having made a complete or nearly complete recovery from their aphasia one year post-stroke6. Recovery may continue over a period of years, although it is likely to be slow and variable. It is estimated that there are 16,000 New Zealanders living with stroke-acquired aphasia5.
Other acquired conditions also impact on communication. These include two motor speech disorders – apraxia (difficulty initiating and executing voluntary movement patterns necessary to produce speech when there is no paralysis or weakness of speech muscles)7 and dysarthria (impaired movement of the muscles used for speech production)8. Apraxia often occurs alongside aphasia (the impaired ability to use or understand language), but this article focuses specifically on aphasia. Of course, many of the communication strategies discussed later will be relevant to all three conditions. Nurses working in aged residential care are more likely to come into regular contact with people with aphasia, but these individuals may be encountered in almost any health care setting.
Social isolation and frustration
Aphasia is more than just difficulty producing or processing language. It’s also about the impact on the individual’s sense of self, relationships with friends and family or whānau, and has to be understood within a wider cultural and social context. Experiences of aphasia that include communication difficulties and the associated frustration, social isolation and depression can’t be separated from the overall impact of the stroke. ‘Ed’ (see introduction) not only lost his speech, but his identity and place in the world9 as well as experiencing significant physical disabilities. He also had no option but to accept admission to aged residential care.
Aphasia can be socially isolating, and the source of much frustration. Tom Gilbert, an American physician, describes the impact of his post-stroke aphasia:
As my recovery progressed, I became aware of how isolated I had become. My inability to process information at a normal speed meant that I had difficulty following conversations and responding in an appropriate manner. My limited speech made it extraordinarily challenging to communicate. For example, my observation that Peggy’s car inspection sticker had expired resulted in 20 minutes of gestures and ’yes‘ and ’no‘ responses before she understood my point. Multiply this exchange by hundreds throughout the day to understand my exhaustion, frustration, and depression. It seemed that my former self was alive and well in a maze inside my brain, leaving only a simpler version of Tom communicating with the outside world10 (p. 202).
While the changes were profound for Tom, his wife also went from being an equal partner to needing to take charge, including making medical decisions for Tom. She also had to assume power of attorney for him.
While family or whānau experience major disruptions in their relationships with a person following a stroke and the development of aphasia, cultural support and social networks can counter some of the impacts of aphasia. Participants in New Zealand research into Māori experiences of aphasia highlighted the centrality of language to all aspects of their world, meaning the loss of language could be considered tragic11.
Both the individuals and their whānau keenly felt the loss of social roles associated with the aphasia, although considerable effort was expended by whānau to ensure the individual’s status was unaffected. While individuals with aphasia in that study experienced negative emotions associated with their condition, they were also able to ‘count their blessings’ because they were grateful for what they still had and were aware it could have been far worse.
Challenges in nursing individuals with aphasia
Nurses are required to communicate effectively with their clients12. Achieving two-way communication may be problematic when language is disrupted, giving rise to feelings of hopelessness and frustration for both the individual and the nurse13.
There are many factors that have the potential to result in challenges for nurses working with people with aphasia. Workload demands can impact on the time available to communicate with individuals, and nurses may also lack the knowledge, skills and confidence associated with facilitating conversations when aphasia is present.
Research has shown that even on specialist stroke wards, nurses engage in nurse-dominated conversations with patients that are largely focused on the nurses’ goals, with more than 54 per cent of interactions related to nursing tasks13. Communication enables the transfer of information, but is also fundamental to the development of social relationships, so essential for safe nursing practice14.
Each practice context presents its own challenges for nurses working with individuals with aphasia. In aged residential care, for example, challenges may include staff turnover, the high proportion of care being delivered by unregulated caregivers, the complexity of other co-morbidities the resident may be experiencing, restricted educational opportunities for staff, and limited access to other health professionals15. Having to communicate with staff for whom English is a second language may also be an additional barrier for residents. Residents’ access to speech-language therapists can also be erratic following the initial rehabilitation period.
Enhancing communication
There is no magic bullet for nurses who wish to improve their communication with individuals with aphasia, in part because of the diversity, extent and combination of symptoms. A broad approach is required, including supporting the person to develop a new sense of self and identifying how best to manage the time pressures associated with nursing workloads. Nurses may also require education on various communication principles/tips, and how to implement these.
Telling our stories (narrative) is an important component of all our lives – helping us to make sense of our world, and who we are within that world. When a person’s sense of self is dramatically disrupted by experiences such as post-stroke aphasia, narrative becomes even more important in helping reconnections between life as it is now and life before the stroke.
Narratives are also a valuable source of service feedback for health care providers14. Hersh14 promotes the need for nurses to become ‘conversation partners’, who can “… assume an active role in supporting, co-constructing and valuing these narratives” (p. 231).
Getting to know the person first, understanding their history and interests, enables new or modified goals to be identified7. Family may be able to provide information to support biographical connections, but nurses should be mindful that individuals and their families or whānau could have different perspectives and understanding of what was important and meaningful.
Nurses may need to seek further education on how best to manage their interactions with individuals with aphasia, such as how to deal with hesitations and silences13. Reflection on and reframing of workload demands is also necessary if appropriate time is to be allocated to ‘getting to know’ the person with aphasia. Hemsley et al16 explored the barriers to and strategies for successful communication between hospital-based nurses and patients with complex communication needs. Nurses who felt time-pressured because of demanding workloads avoided direct interactions with patients and relied instead on communication with family or paid carers.
Perceptions that communication difficulties may reflect intellectual disability, even when that is not the case, also discouraged nurses from investing time into communicating with the patient.
Conversely, in the same study, there were nurses who took the time to understand the patient’s point of view, were prepared to use a range of adaptive strategies to facilitate communication, and were open to the potential success of that communication. As those nurses noted, ‘being patient’ not only enhances wellbeing for the patient but also saves time in the long run. Communication becomes easier with the passage of time, and the nurses became more familiar with non-verbal expressions and responses.
When individuals with aphasia are transferred to aged residential care facilities from a stroke unit, nurses should ensure they access any communication books or strategies initiated by speech and language therapists for that individual.
Numerous websites contain ‘communication tips’ for working with individuals experiencing aphasia. Many of these tips, such as not talking over the person, should be fundamental communication practices; however, a reminder is always useful. Common suggestions include:
- Minimise background noise.
- Speak clearly and not too quickly.
- Listen attentively.
- Use short, clear sentences, giving one piece of information at a time.
- Clarify and rephrase when necessary.
- Take time to allow the person to respond, and time for rests if necessary.
- Use facial expression, tone of voice, and gestures to explain.
- Encourage the person to let you know when they haven’t understood.
- Have pen and paper available for both parties.
- Write down key words.
- Ensure appropriate communication devices and material are available (i.e. applications on electronic devices, individualised picture books and alphabet boards).
(adapted from Aphasia Alliance17)
Box 1
The range of aphasia symptoms
“Aphasia can be so severe as to make communication with the patient almost impossible, or it can be very mild. It may affect mainly a single aspect of language use, such as the ability to retrieve the names of objects, or the ability to put words together into sentences, or the ability to read. More commonly, however, multiple aspects of communication are impaired, while some channels remain accessible for a limited exchange of information.”
National Aphasia Association2
Conclusion
For some individuals who develop aphasia, the experience may be temporary or of minor consequence. For others the impacts of aphasia can be profound, both for the person themselves, but also their wider family or whānau. As with any major disruption to health status, lives are rewritten and new ways of being must be developed. Skilled and compassionate nursing can help those affected regain communication skills and a new place in the world.
View PDF of this learning activity here >>
Recommended resources
- The Aphasia Simulations website includes a useful overview of aphasia, communication tips, and a number of short simulations that provide a sense of what a person with aphasia may be experiencing. http://aphasiacorner.com/aphasia-simulations/index.html
- The Tavistock Trust for Aphasia website contains links to a range of resource information, including information on finding assistive technologies for people with aphasia. www.aphasiatavistocktrust.org/aphasia/what-is-aphasia
- Krishna Pindolas’s blog ‘My battle against my stroke’ describes her experiences, which included aphasia, after a stroke at the age of 18. http://strokerecoverybc.ca/newsletter/battle-stroke-krishna-pindolias-blog
- If you would like to know more about the different types of aphasia, check out aphasia definitions on the National Aphasia Association’s website www.aphasia.org/aphasia-definitions. The association has also produced an 18-minute video entitled ‘Patience, communication and understanding’ (2013). This provides a moving insight into the experiences of a small group of adults with a range of aphasia symptoms and includes strategies to aid effective communication. www.youtube.com/watch?v=aPTTjRTmgq0
- Hersh (2012, full details in reference 14) provides several interesting examples (for example, p. 227) of how an expert communicator can facilitate explicit narratives with individuals with aphasia.
- There are numerous videos on YouTube of experiences of aphasia, such as a series of videos made over a six-year period by Sarah Scott, who developed expressive aphasia after a stroke when she was 18 years old. This is the link to the first of her videos: www.youtube.com/watch?v=1aplTvEQ6ew.
About the authors
- Marian Bland RN PhD is the quality coordinator at Ranfurly Residential Care Centre, Feilding and a health care auditor.
- Lesley Batten RN PhD is a senior researcher at Massey University, Palmerston North.
This article was peer reviewed by:
- Julia Slark RN PhD, senior lecturer at the University of Auckland
- Olivia Browne RN, stroke clinical nurse specialist at Hutt Valley District Health Board
References
- Personal anecdote of MB
- NATIONAL APHASIA ASSOCIATION (n.d.) Aphasia definitions www.aphasia.org/aphasia-definitions
- STROKE FOUNDATION OF NEW ZEALAND (N.D.) Facts and fallacies. www.stroke.org.nz/stroke-facts-and-fallacies
- STROKE RECOVERY ASSOCIATION OF BRITISH COLUMBIA (2017) Learn more about aphasia.
http://strokerecoverybc.ca/7-steps-guide/aphasia-guide/ - APHASIA NZ CHARITABLE TRUST (2010) Aphasia facts. www.aphasia.org.nz/public/about/public-about
- POSLAWSKY I, SCHUURMANS, M, LINDEMAN E & HAFSTEINSDOTTIR T (2010) A systematic review of nursing rehabilitation of stroke patients with aphasia. Journal of Clinical Nursing 19, 17-32.
- AMERICAN HEART ASSOCIATION/AMERICAN STROKE ASSOCIATION (2013). Aphasia vs apraxia. http://goo.gl/1mMnRY
- AMERICAN SPEECH-LANGUAGE ASSOCIATION (2016) Dysarthria. www.asha.org/public/speech/disorders/dysarthria
- THOMPSON J & MCKEEVER M (2012) The impact of stroke aphasia on health and well-being and appropriate nursing interventions: An exploration using the Theory of Human Scale Development. Journal of Clinical Nursing 23, 410-420.
- GILBERT T, GILBERT M, CULPEPPER L & WILKINSON, J (2013) Voices of recovery: A family physician’s experience of aphasia. Family Medicine 45(3), 201-204.
- MCLELLAN K, MCCANN C, WORRALL L & HARTWOOD M (2014). “For Māori, language is precious. And without it we are a bit lost”: Māori experiences of aphasia. Aphasiology 28(4) 453-470.
- NURSING COUNCIL OF NEW ZEALAND (2012) Competencies for registered nurses. Retrieved January 2016 from www.nursingcouncil.org.nz/Publications/Standards-and-guidelines-for-nurses
- GORDON C, ELLIS-HILL C & ASHBURN A (2009) The use of conversational analysis: Nurse-patient interaction in communication disability after stroke. Journal of Advanced Nursing 65(3) 544-553.
- HERSH D (2015) “Hopeless, sorry, hopeless”: Co-constructing narratives of care with people who have aphasia post-stroke. Topics In Language Disorders 35(3), 219-236.
- CARRYER J, HANSEN C & BLAKELY J (2010) Experiences of nursing in older care facilities in New Zealand. Australian Health Review 34, 11-17.
- HEMSLEY B, BALANDIN S & WORRALL L (2011) Nursing the patient with complex communication needs: Time as a barrier and a facilitator to successful communication in hospital. Journal of Advanced Nursing 68(1) 116-126.
- APHASIA ALLIANCE (2014) Top tips for ‘Aphasia Friendlier’ communication. Retrieved on 26 March 2016 from www.aphasiaalliance.org/top-tips
This learning activity is relevant to the Nursing Council competencies 1.4, 2.2, 2.3, 2.4, 2.6, 2.7, 2.9, 4.1 and 4.3
Learning outcomes:
Reading and reflecting on this article will enable you to:
- update your knowledge on serious drug allergies as a subset of adverse drug reactions
- identify your responsibilities in the nursing care of a person with a risk of drug allergies
- reflect on medication safety practices in your workplace and identify whether any improvements are required related to preventing drug allergies.
Introduction
As the emergency department nurse starts the first dose of an IV antibiotic infusion, she asks, “You’re not allergic to anything are you?” I reply, “Yes, I’ve a long list of serious drug allergies – all in my notes”. She leaves the infusion running, and with no call bell I sit and wait, wondering if and when I might react to this drug. I have no sense the nurse understands how dangerous a delayed hypersensitivity reaction can be, even after my description of weeks in hospital following one such reaction1.
Adverse drug reactions (ADRs) are common, and for patients who experience an ADR, that experience can be distressing, painful, and one that they revisit every time they are prescribed another medication.
About 80 per cent of ADRs are classified as Type A reactions, which are predictable and dependent on the drug dose (Table 1). About 15–20 per cent of ADRs are Type B reactions, which are unpredictable and independent of the dose2,3.
It is this last group of drug reactions, specifically the immunologically mediated reactions, that are the focus of this article. Although categorised as ‘unpredictable’, there is much nurses can do to prevent patient harm from these reactions.
It’s not all about anaphylaxis
While many patients report drug allergies, the true incidence is unknown3. It is complicated by a number of factors, including:
- skin symptoms such as rashes can be related to other conditions, for example infections, rather than to an allergy4
- patients often report or self-diagnose ‘allergies’ to drugs, when that diagnosis may not have been confirmed
- patients report another category of reaction, such as a recognised side effect, as an allergy. Think about how often patients report nausea as an allergy symptom.
Therefore, identifying allergies and ADRs requires careful assessment and identifying an allergic reaction as the source of symptoms may not be straightforward.
Nurses learn about anaphylaxis, but that is only one of a number of types of potentially fatal allergic reactions to medications. Other serious reactions that result from different immune responses are now categorised as types of severe cutaneous adverse reactions (SCARs)3 (see tables 2 and 3).
Drugs are one of the major causes of these relatively rare and idiosyncratic syndromes. For example, between 1965 and 2004 the New Zealand Centre for Adverse Reactions Monitoring (CARM) received 585 reports of SCARs associated with medicines or vaccines5. At that time CARM identified the antibiotic Cotrimoxazole as responsible for 77 SCAR reports5, while more recently NSAIDs have been associated with 41 case reports6. SCARs can cause significant morbidity, including blindness and disfigurement and, depending on the syndrome, have a mortality rate of 5–40 per cent7. Any treatment can be difficult and protracted.
It was one of these SCAR reactions that resulted in the widely reported death of New Zealander Eunice Richardson in 2013. Mrs Richardson was prescribed and given Trimethoprim, even though she had had a previous severe reaction to this medication8. In this tragic case both her MedicAlert® bracelet and written warnings of her allergy status on all pages of her clinical record were insufficient protection for her, with fatal consequences8. (See link to video and exercise in the Recommended Resources’ section.)
TABLE 1:
| Type A reactions –
predictable & dose dependent (~80% of ADRs) |
Type B reactions –
unpredictable & dose independent (~15-20% of ADRs) |
| • Overdose
• Side effects, e.g. gastrointestinal bleeding with non-steroidal anti-inflammatories [NSAIDs], • Secondary effects • Drug-drug interactions e.g. Erythromycin + Warfarin = potential increase in blood drug levels |
· Drug intolerance, e.g. tinnitus with aspirin
· Drug idiosyncrasy · Pseudo allergic reactions · Immune-mediated drug hypersensitivity reactions
|
The ‘anatomy’ of an adverse event
In every adverse event, such as Mrs Richardson’s case and in the personal experience recounted at the start of this article where the nurse didn’t check the allergy status before preparing a drug for administration, there is a multitude of potentially contributing factors. Some factors are organisational; for example, clinical record policies. Others are situational, such as interruptions during the drug administration processes and heavy nursing workloads.
Investigations of adverse events often find that a nurse’s mistaken belief that they ‘know the patient9, is a contributing factor. In those circumstances the usual checking of allergy details – when a drug is prescribed and about to be administered – can be missed and cues, such as a MedicAlert® bracelet, overlooked.
The New Zealand Health Quality and Safety Commission currently has a National Medication Safety Programme underway aiming to reduce preventable harm from medication errors and adverse drug events, including drug allergies. This multifaceted safety programme includes the development of the national medication chart and raising awareness of medication risks. Additional work, following the case of Mrs Richardson, has been the distribution of a ‘safety signal’ to New Zealand health professionals about risks of serious adverse drug reactions, including ways to reduce risks10,11.
The key to reducing risk is to identify that prevention is possible.
Preventing or minimising SCARS (and other drug allergies)
Although some allergic reactions to drugs cannot be prevented or foreseen, there is much that nurses can do to minimise the impacts of these severe adverse reactions:
Don’t overlook blank or incomplete allergy and adverse drug reaction information
Adverse drug reaction information can be obtained from multiple sources, including patients, the family or whānau, carers, clinical records, the national medical warning system and MedicAlert®. A blank space in the allergy and adverse drug reaction section on a clinical record should be a red flag to nurses that the chart is incomplete and needs updating.
“Taking a medication history is an integral part of any patient’s diagnosis or treatment. Within that history, it is important to find out if the patient has had any previous allergies or adverse drug reactions and what the reactions were, as these can influence clinical decisions. The patient’s clinical records, whether paper or electronic, should be checked for this information” 11.
Just as important as this process of checking is making sure that any new reactions are diagnosed, and documented thoroughly, including on transfer and discharge summaries11. Patients need to be given accurate information about that reaction and the steps they should take to prevent future reactions. This is the time to talk to patients about applying for a MedicAlert® bracelet, or updating their MedicAlert® records.
Table 2: Categorisations of reactions
| Severe cutaneous adverse reactions (SCAR) syndromes3 | |
| SJS/TEN | Steven Johnson syndrome/ Toxic epidermal necrolysis |
| DiHS/ DRESS | Drug-induced hypersensitivity syndrome/Drug rash with eosinophilia and systemic symptoms |
| AGEP | Acute generalised exanthematous pustulosis |
Table 3: Immune-mediated reactions
| Types of immune-mediated adverse drug reactions2, 7, | ||||
| Hypersensitivity reaction | Mechanism | Examples | Symptoms may include | Symptoms may start after drug commenced- immediate or delayed |
| Type I
|
Immunoglobulin E-mediated | Anaphylaxis, angioedema & urticaria | E.g. hypotension, urticaria, laryngeal oedema, bronchospasm | Immediate (minutes to hours) |
| Type II | Immunoglobulin M or G-mediated (tissue-specific) | Haemolytic anaemia & organ-specific reactions | Depends on the tissue, e.g. anaemia or thrombocytopenia | Immediate or delayed |
| Type III | Immune complex-mediated | Serum sickness & drug fever (delayed) | Fever, lymphadenopathy, urticaria, arthralgia, other rashes | 1-3 weeks |
| Type IV
SCAR syndromes |
Cell-mediated
(T-cells) |
SJS/TEN | Epidermal detachment, purpuric macules, mucosal lesions and kidney, liver, eye & lung involvement,
fever and malaise |
1-8 weeks |
| DRESS/DiHS | Facial oedema, fever, eosinophilia, plus lymphadenopathy, hepatitis, lung, kidney, thyroid and myocardial inflammation in some cases | 3-12 weeks | ||
Ask patients and their whānau to ‘speak up’ about their allergies
A research project – during which all patients were given a questionnaire about drug allergies and were asked to ‘speak up’ about previous reactions – resulted in a significant increase in documented allergy information. This process also provided nurses with greater opportunities to clarify with patients whether their reactions were minor side effects or allergic reactions, and to then establish if this information has been entered on the patient management system12.
Ask a pharmacist to do a medication review
With their specialist knowledge of drugs and cross sensitivities pharmacists are well placed to review prescriptions, reported drug allergies, and also to review drug allergies recorded under a patient’s National Health Index number.
“I had a reaction to a cough syrup with Actidil in it. Years later I had a bad reaction to Benadryl. I didn’t know I could be allergic to an antihistamine so I talked to a pharmacist, who told me the drugs were related. No doctor or nurse had ever told me that1.”
Know the patients most at risk of a drug allergy
Genes play a part for some patients who have serious drug allergies, however genetic testing is not commonly used in clinical practice. However, nurses can be alert to:
- Specific drugs more likely to cause allergic reactions, such as chemotherapeutic agents3
- ‘Allergic’ patients, those who have had a previous drug allergy, and especially those with multiple allergy syndrome, who have reacted to more than one type of drug in the past2
- Specific concurrent medical conditions, including patients with Epstein-Barr virus, HIV, asthma, malignancy, autoimmune disorders, and immune compromised patients3.
Recognise and act on early signs
Not all reactions are immediate. SCAR syndromes can take between one to eight weeks before symptoms occur, even developing after the drug has been discontinued (table 2). Symptoms often last for weeks, even with supportive treatments, or may even become permanent. Therefore, consider allergies if a patient reports new symptoms after a drug has been administered or discontinued. Importantly, the prognosis in SCAR cases can be improved by stopping the suspected medication as soon as possible5. Therefore, know your local policy for withholding a medication dose and reporting a suspected allergy.
Report inadvertent prescribing or administration of drugs to ‘allergic’ patients
Even if no reaction occurs, report any instances where drugs are prescribed to a patient known to be allergic to those medications. These incidents should be analysed to prevent future cases.
Acknowledge the limitations of the ‘five rights’
The five rights of safe drug administration (right patient, time, drug, dose, and route)
do not overtly include provision for checking patient histories for drug allergies13. Nurses can help prevent adverse reactions by having a comprehensive knowledge of the drugs they may prescribe and administer, and good patient knowledge to identify those most at risk. Other responsibilities include reporting drug reactions to CARM, which can update details in the patient’s records via their National Health Index number through the Medical Warning System. It is also important that nurses know and follow their district health board and organisational adverse drug reaction policies, which will provide details on local policies. This will include, for example, the use of coloured stickers on clinical records, additional allergy bracelets, and entries in the patient management system.
Conclusion
Any of us can have an adverse drug reaction; however, some reactions can be prevented by good prescribing and drug administration practices, including knowing which patients are most at risk and which drugs are the most likely culprits. Nurses need to understand the types of drug reactions so that they can help patients differentiate between known side effects and allergies, can spot early symptoms, and can provide appropriate care for patients who have reactions. That care includes ensuring steps are taken to reduce future allergic reactions to medications.
Ask your patients about their drug allergy history, listen to what they say, document carefully, and remember SCARs are much more than skin deep and can kill, but also remember that many of those serious reactions can be prevented.
View PDF of this learning activity here >>
Recommended Resources
The Health Quality And Safety Commission New Zealand provides details in its user guide on correct use of the National Medical Chart and specifically the documentation of allergies and adverse reactions: National medicationchart user guide (2nd edition). www.hqsc.govt.nz/assets/Medication-Safety/NMC-PR/NMC-UserGuide-Aug-2015.PDF
Greater detail on the physiology underpinning drug allergies can be found on YouTube, with Ashley Khan’s presentation ‘But I’m allergic to that… a closer look at drug allergies’: www.youtube.com/watch?v=rh15FhXwzQE
The United Kingdom National Institute For Health And Care Excellence provides an excellent guideline: Drug allergy: diagnosis and management. NICE guideline [CG182]. www.nice.org.uk/Guidance/CG183
The Press: Watch the two-minute interview with the husband of drug allergy victim Eunice Richardson, in which he recounts his experience. Note down all of the times when this fatal reaction could have been prevented. www.stuff.co.nz/the-press/news/69258944/allergic-reaction-to-antibiotic-medication-kills-woman
About the authors:
- Lesley Batten RN PhD is a senior researcher at Massey University, Palmerston North.
Marian Bland RN PhD is the quality coordinator at Ranfurly Residential Care Centre, Feilding, and a health care auditor.
This article was peer reviewed by:
- Kathleen Brown RN MN is an NP in lifespan acute care working in Palmerston North’s Central City Medical Centre.
Anecita Gigi Lim RN PhD is a senior lecturer at The University of Auckland’s school of nursing, teaching nurse prescribing and pharmacology.
References
- Personal anecdotes of LB
- BLUMENTHAL K, SAFF R, & BANERJI A (2014) Evaluation and management of a patient with multiple drug allergies. Allergy and Asthma Proceedings 35 197-203.
- THONG B, & TAN T (2011) Epidemiology and risk factors for drug allergy. British Journal of Clinical Pharmacology 71(5) 684-700.
- HEINZERLING L, TOMSITZ D, & ANLIKER M (2012) Is drug allergy less prevalent than previously assumed? A 5-year analysis. Epidemiology and Health Services Research 166, 107-14.
- MEDSAFE: NEW ZEALAND MEDICINES AND MEDICAL DEVICES SAFETY AUTHORITY. (2005). Severe cutaneous adverse reactions: More than skin deep. Prescriber Update 26(2) 28-29.
- MEDSAFE: NEW ZEALAND MEDICINES AND MEDICAL DEVICES SAFETY AUTHORITY. (2012) NSAIDs can SCAR (Severe Cutaneous Adverse Reaction). Prescriber Update 33(2) 11-12.
- MAROTTI M (2012) Severe cutaneous adverse reactions (SCAR) syndromes. Revista da Associacao Medica Brasileira 58(3) 276-278
- THOMAS, R (2015, June 12) Hospital warned about Eunice Richardson’s allergy before fatal mishap. The Press www.stuff.co.nz/the-press/news/69341672/hospital-war
- DOUGHERTY L, SQUE M, & CROUCH R (2012) Decision-making processes used by nurses during intravenous drug preparation and administration. Journal of Advanced Nursing 68(6) 1302-1311.
- HEALTH QUALITY & SAFETY COMMISSION NEW ZEALAND. (2015, September) Safety signal: The risk of serious adverse drug reactions. Retrieved January 2016 from www.hqsc.govt.nz
- HEALTH QUALITY & SAFETY COMMISSION NEW ZEALAND (2015, 14 September) Medical ID bracelet incident timely med safety reminder. Retrieved January 2016 from www.hqsc.govt.nz/our-programmes/medication-safety/news-and-events/news/2303
- VALENTE S, MURRAY L, & FISHER D (2007) Nurses improve safety with medication allergy and adverse drug reports. Journal of Nursing Care Quality 22(4) 322-327.
- GEORGE E, HENNEMAN E, TASOTA F (2010) Nursing implications for prevention of adverse drug events in the intensive care unit. Critical Care Medicine 38(6) S136-144.
- NURSING COUNCIL OF NEW ZEALAND (2012). Competencies for registered nurses. Retrieved January 2016 from: www.nursingcouncil.org.nz/Publications/Standards-and-guidelines-for-nurses
This learning activity is relevant to the Nursing Council competencies: 1.2, 1.4, 1.5, 3.2, 4.2
Learning outcomes
Reading and reflecting on this article will enable you to:
- Consider the impact of institutional visiting hours on patients, their family or whānau
- Reflect on your personal and professional response to visitors in your work area
- Compare staff responses to visiting in your own work area
- Formulate strategies that will allow you to effectively manage and maintain the safety of patients and staff, while still maintaining a partnership approach that values the input of families and whānau.
Introduction
As I was pushing my niece in a wheelchair to see her new premature baby the day after her emergency caesarean section, the unit receptionist asked who I was. Her response to that information was to tell me I could visit this time (as I was pushing the wheelchair), but in future would have to wait for visiting hours. She then recited the visiting rules. What a welcome, and not what my niece needed at that time1.
Visiting hours in New Zealand’s public hospitals have been a moveable feast over recent decades. While the rules around visiting may be becoming more accommodating, restrictions remain in many parts of the country with a significant variation in official visiting hours between DHBs.
Although restrictions in hospital visiting may follow historical precedents2, it is often difficult to identify the rationale behind current restrictions. The most common explanation found on DHB websites was the need to allow patients to rest. Other reasons included:
- Increased staff workload, which is then disrupted by visitors
- Lack of space
- Patients requiring treatments
- Privacy issues associated with medical rounds
- Visitors being inconsiderate to other patients
- Concerns about theft and vandalism, especially after hours
- Cross-infection.
These reasons link to broader concerns about maintaining a safe environment for staff, patients and other visitors. In 2010, Waikato Hospital was reported as being about to trial new restricted visiting hours in response to what they referred to as “chaotic, overcrowded wards” in the hope of “regaining control” over patients’ recoveries3. In late 2014, an unnamed staff member at Whanganui Hospital claimed in the media that nurses feared for their safety at the hospital because of a lack of control over what were described as “volatile” visitors4. While these concerns are real for the staff concerned, are restrictions on visiting always the answer or are they sometimes the problem?
Applying the rules
Even within the one hospital there can be considerable variation in visiting hours between wards and units, as well as
differences between institutions in the same DHB. Regardless of what the official visiting hours may be, inconsistencies in adherence to those hours are common and problematic for everyone. At a ward/unit level, some staff may be prepared to put patients’ needs ahead of the policy, as the following anecdote demonstrates:
I was the identified support person for a close friend recovering from extensive abdominal surgery. My friend was deeply shocked by her diagnosis, as well as recovering from the surgery. She wanted somebody with her constantly to support her for the first few days post-op. The ward was closed to visitors for several hours each afternoon. Some nurses were quite comfortable with me reading quietly in her room, as long as I didn’t disturb her rest or that of any other patient. Other staff were sticklers for pushing everyone out the door and locking it fast1.
Working out whether staff are ‘sticklers’ or not puts additional stress on patients and families who have to decipher the rules5. Having to plead for access out of hours can be demeaning for visitors, and patients may be left distressed:
I was scared that I was going to die because of my previous reaction to Fentanyl. My husband knew, my mother knew, but they weren’t there. That terrifying situation happened because the hospital’s rules wouldn’t allow my family to stay with me6.
Not only was this patient distressed, but it is likely that her family were also discomforted – wanting to be there, knowing they should be there and not being allowed. This raises the issue of whether ‘visitor’ is even the correct term for family members, whānau or significant others?
Visitor status
I’d been staying with Mum in hospital, showering her, taking her to the toilet, doing whatever she needed. The nurses watched her drip. We have a pākehā friend who is like family to us. Mum calls her ‘her other daughter’. I’d been there for three nights, and was exhausted, so my ‘sister’ took over being with Mum for the night shift. I told the nurse I was going home, and that my sister would be with her. I rang later to check how Mum was, and the nurse said, “Oh, you are supposed to be up here with your mother”. I asked if anyone was with Mum, and she replied, “There’s a blonde person sitting out there with her”. That doesn’t sound very nice, does it7?
In this situation, staff were comfortable with family members being present 24 hours a day, and undertaking much of their mother’s personal care. Unfortunately, assumptions were made based on cultural stereotypes about who could be a whānau member, and without understanding that a kaupapa whānau includes others not related by kinship.
Contemporary families are complex and diverse and it is always dangerous to make assumptions as to who is the most significant patient supporter, or to attempt to determine ethnic identity on the basis of physical characteristics.
One useful approach is to adopt personcentred visiting, where the patient and their family decide who are the significant people to be present when someone is in hospital.
Use of a ‘nominated contact person’ or ‘identified support person’ goes some way in enabling patients and family to identify significant supporters, but the missing component is free access to provide the necessary support.
Box 1: Family presence and participation
Restrictive visiting policies are often based on long-held beliefs that the presence and participation of families interferes with care, exhausts the patient, is a burden to families, or spreads infection. These are myths and misperceptions. There is no current evidence to support those beliefs5
Working in partnership?
As Taima Campbell, the then Director of Nursing and Midwifery for the Auckland DHB, noted in 2012: “On the one hand we talk about patient-centred care; for a lot of patients, part of their healing is having their family. On the other hand, we kick [families] out.8”
Restricting visiting not only limits family access to the patient, it also reduces the important opportunities for staff and families to interact. Restricting opportunities for families to communicate with staff conflicts with nurses’ professional and legal responsibilities to work in partnership with the patient and their family (refer to related competencies and standards sidebar).
The New Zealand Health Quality and Safety Commission9 recently published the results of its survey of 6,000 people who were inpatients in DHB hospitals in November 2014. Only 55 per cent of respondents reported that the hospital staff included their family or whānau or someone close to them in discussions about their care.
The people who are essential to the ongoing support, comfort, and wellbeing of the patient must be identified and included. As argued by Clisset et al10 in a study of the experiences of family carers of older people with mental health problems who were admitted to general hospital wards: “Health care professionals need to be more consistent in working in partnership with family carers, recognising them as a source of expertise in the specific needs of a person …” This theme of the need for nurses and families to work in partnership recurs in the literature supporting open visiting policies11.
Cultural considerations
The need for families to be present when a family member is sick is an almost universal cultural value5. The configuration of our public hospitals poses some challenges in relation to person-centred visiting. Our older hospitals
have a predominance of shared rooms, where four-bedded cubicles are common, patient privacy is at a premium, and small, uninviting patient lounges provide limited opportunities for visiting family groups. These environmental factors create problems for nurses, and also for families:
My uncle was in hospital, and all the whānau came in to see him because that’s what he wanted and expected. He had many visitors, and there wasn’t enough space in his room so others were waiting quietly in the lounge. Just feeling those vibes from staff like ‘you shouldn’t be here, there are too many of you in there’. I was feeling a bit stressed out ‘cause they were all looking at us, but uncle didn’t want us to go. They had their rules, even down to the numbers of visitors he was allowed, but those rules were a problem for uncle, and therefore for us7.
In this example, space for a large whānau caused challenges, however so did the style of communication between nurses and the whānau. The whānau were the ones caughtbetween the rules, the patient’s need for family support, and the whānau obligations to care. The importance of the whānau to patient recovery is well recognised12. While some new hospitals now include visitor lounges/rooms to accommodate larger family groups, these are not available in all hospitals, however they should be prioritised.
Box 2: The presence and participation of families/other partners in care
- Families and other partners in care welcome 24 hours (as determined by patient preference)
- Patients asked to define family/partners in care, and with the guidance of staff determine what their role will be
- Negotiation about the number of people who can be at the bedside at any one time
- Expectations for when children visit
- Identification of a family spokesperson
- Directly and promptly addressing disruptive behaviour
- Visitors free from infection
- During disease outbreaks, staff work to facilitate selected family members still being present.
Extract from guidelines developed by the Institute for Patients and Family-Centred Care (19).
Open all hours?
Research has identified the impact on patient outcomes when family members are present, including benefits such as a reduction in patient falls6. In one of the few randomised trials comparing restricted with unrestricted visiting in an intensive care unit13, researchers identified positive outcomes for patients when visiting was unrestricted including reduced anxiety scores, lower levels of stress hormones, reduced cardiovascular complications, and no increase in sepsis. The National Health Service Scotland has produced a short film celebrating the many positive effects resulting from their implementation of person-centred visiting14.
This includes family support when staff are busy, staff gaining an increased understanding of the patient’s background, and improved safety and effectiveness of care. They note that when visitors are not constrained to
specific short periods of visiting, they are much more likely to leave when the patient is tired, knowing they can come back again later. In many overseas countries, families are expected to be present 24 hours a day to provide all of the personal cares that a patient requires. In New Zealand’s professionalised health care system, the roles of families in providing care have changed, but staff then frequently report they are unable to provide such care because they are too busy15. There are opportunities for enhancing nursing roles when families who are able are supported to take responsibility for activities such as ensuring the patient is assisted at meal times. However, ongoing communication between the staff, patients and family members about caregiving roles is crucial for safe care16. In organisations where open visiting is supported, additional responsibilities have been identified for nurses, including transitioning from patientcentred to family-centred care and caring for family members16. With person-centred visiting, there are few, if any, restrictions on the hours during which visitors may be present. However there are guidelines to maintain a safe environment and a core component is the need for communication between all parties.
Ensuring the safety of visitors during emergency situations must also be considered. The evidence from institutions that have moved to this system is that it has been positive for patients, families and staff14,17,18,19 although a formal change management process is essential for success.
Clear guidelines are necessary to ensure patient, visitor and staff safety. These may include:
- Patients and families nominating who is to have unlimited access
- Guidance about supporting patient recovery through rest periods
- Acceptance by families that staff may require them to leave temporarily when treatments are being undertaken
- Emergency management plans also include strategies to support family/visitors present at the time of an emergency
- Appropriate security arrangements, especially after hours, when there are fewer staff present
- Adequate space for visitors to avoid disturbing other patients
- Consistent communication with patients and families via information from staff, appropriate signage, and information booklets.
Conclusion
Restricting visiting hours limits the opportunity for working in partnership with patients and their family or whānau. Reconsideration of what constitutes visiting, and who visitors are, is long overdue. One perspective worthy of further consideration is the notion that it is hospital staff who are visitors in the patients’ lives, rather than their families being visitors in the life of the hospital6. Changes in attitudes, policy and practice, and most importantly, communication, are required to ensure that the visiting experience is a positive one for the patient, their family/whānau and all members of the health care team.
View PDF of this article (and related learning activity) here >>
About the authors:
- Lesley Batten, RN PhD and Marian Bland, RN PhD are both experienced nurses and researchers, and regular hospital visitors supporting hospitalised family and friends.
- Lesley works in the Research Centre for Māori Health & Development, Massey University, Palmerston North. Marian is Quality Coordinator, Ranfurly Residential Care Centre, Feilding, and a health care auditor.
This article was peer reviewed by:
- Denise Wilson RN BA MA (hons) PhD (Nursing) is Professor of Māori Health and director of the Taupua Waiora Centre for Māori Health Research at Auckland University of Technology.
- Sue Wood RN MNS is the former director of nursing for MidCentral District Health Board and currently Quality & Patient Safety Director for Canterbury District Health Board.
Recommended resources
- The American Joint Commission on Healthcare website has resources on effective communication and cultural competence related to family-centred care: www.jointcommission.org/Advancing_Effective_Communication
- Better Together: Partnering with Families is an initiative of the American Institute for Patient and Family-Centred Care: http://www.ipfcc.org/bestpractices/better-together.html
- White Coat, Black Arts is a Canadian radio programme discussing various aspects of visiting hours, the restrictions imposed when patients are in shared rooms, and the consequences for the family of a terminally ill patient: www.cbc.ca/radio/whitecoat/the-end-of-visiting-hours-1.2801166
- Health Safety and Quality Commission New Zealand outlines a number of strategies for getting feedback from health consumers about services: https://www.hqsc.govt.nz/our-programmes/partners-in-care/publications-and-resources/publication/784/
Health and Disability Sector (Core) Standards 200821
Standard 1.12 Consumers are able to maintain links with their family/whānau and their community.
Criteria 1.12.1 Consumers have access to visitors of their choice.
Guidance: Consumers have access to visitors of their choice (including children) when the safety of the consumer and others is not compromised. The safety of consumers in the presence of visitors needs to be assured. This may include, but is not limited to:
- Clinical stability of consumer
- Legal status of consumer
- Safety in relation to room size and/or other consumers in a shared room
- Appropriate behaviour of visitors – such as behaviours that impinge on the safety of the consumer, other consumers,and/or service providers
REFERENCES
- Personal anecdotes freely shared with the authors about visiting in New Zealand hospitals when people heard they were developing this article.
- ISMAIL S & MULLEY, G (2007). Visiting times. British Medical Journal 335 1316.
- TWENTYMAN, M (2010). ‘Chaotic’ hospital targets visiting times. Waikato Times 28 August, A9.P
- Nurses fear for safety. Hawke’s Bay Today, 13 December 2014, A017.
- CIOFFI, J (2006). Culturally diverse family members and their hospitalised relatives in acute care wards: a qualitative study. Australian Journal of Advanced Nursing 24(1) 15-20.
- BETTER TOGETHER: PARTNERING WITH FAMILIES (undated). Facts and figures about family presence and participation. http://www.ipfcc.org/bestpractices/Better-Together-Facts-and-Figures.pdf
- BATTEN L, HOLDAWAY M & THE LCP RESEARCH TEAM (2012). Data excerpts from the unpublished study. Culturally appropriate end-of-life care for Māori. Palmerston North: Research Centre for Māori Health and Development, Massey University.
- CASSIE, F (2012). Patients as best teachers. Nursing Review 12(9), 26.
- NEW ZEALAND HEALTH QUALITY & SAFETY COMMISSION (2015). Patient experience results. Retrieved February 2015 from www.hqsc.govt.nz/assets/Health-Quality-Evaluation/NEMR/patient-experience-survey-results-Feb-2015.pdf
- CLISSETT, P, POROCK, D, et al. (2013). Experiences of family carers of olderpeople with mental health problems in the acute general hospital: a qualitativestudy. Journal of Advanced Nursing 69(12) 2707-2716.
- TRUELAND, J (2014). A flexible approach in Scottish hospitals is makingvisitors feel welcome on the wards. Nursing Management 21(2) 8-9.
- WILSON, C, & BAKER, M (2012). Indigenous hospital experiences: A NewZealand case study. Qualitative Health Research 22(8) 1073-1082.
- FUMAGALLI, S, BONCINELLI, L, et al. (2006). Reduced cardiocirculatory complications with unrestrictive visiting policy in an intensive care unit. Circulation 113 946-952.
- NATIONAL HEALTH SERVICE SCOTLAND (2014). Person-centred visiting in NHS Scotland. FILM. Retrieved February 2015 from http://www.qihub.scot.nhs.uk/video-hub/-person-centred-visiting-in-nhsscotland.aspx
- CARVILLE, O (2014). Overworked nurses ration patient care. The Press, 27May, Retrieved February 2015 from www.stuff.co.nz/the-press/news/10079520/Overworked-nurses-ration-patient-care
- RICCIONI, L, AJMONE-CAT, C et al. (2014). New roles for healthcare workers in theopen ICU. Trends in Anaesthesia and Critical Care 4 182-185.
- SHULKIN D, O’KEEFE, T et al. (2013). Eliminating visiting hour restrictions inhospitals. Journal for Healthcare Quality 36(6) 54-57.
- NUSS, T, KELLY, K et al (2014). The impact of opening visitation access on patientand family experience. The Journal of Nursing Administration 44(7/8) 403-410.
- INSTITUTE FOR PATIENT AND FAMILY CENTRED CARE (2015). IPFCC challenges hospitals to eliminate restrictive visiting policies. Retrieved February 2015 from http://www.ipfcc.org/bestpractices/better-together.html
- NURSING COUNCIL OF NEW ZEALAND (2007). Competencies for registerednurses. Retrieved February 2015 from www.nursingcouncil.org.nz/Publications/Standards-and-guidelines-for-nurses
- STANDARDS NEW ZEALAND (2008). Health and Disability Service Standards. Retrieved February 2015 from http://www.health.govt.nz/our-work/regulation-health-and-disability-system/certification-health-care-services/services-standards
Reading this article and undertaking the learning activity is equivalent to 60 minutes of professional development.
Do you or don’t you?
The 2013 influenza season is upon us in the southern hemisphere, and with it, health care workers are faced with the decision about whether or not to receive the seasonal influenza vaccination. For many, the decision to get vaccinated is ‘a given’ as they rationalise it is part of their professional obligation to keep themselves fit for work; as well as to protect their patients. This rationalisation is shared and recommended by the World Health Organisation (WHO)1. Others view getting vaccinated as unnecessary and too fraught with doubts to be considered a viable option to boost their immunity.
Despite slight increases in the flu vaccination uptakes rates by the New Zealand health workforce in the last three years, actual immunisation numbers remain low. The Ministry of Health’s 2012 (MOH) data revealed that only 48 per cent of District Health Board health care workers were vaccinated for influenza and the figure was lower again for DHB nurses at 46 per cent (6). Virologist and National Influenza Specialist Group spokesman Lance Jennings said this year that nurse vaccination levels still needed to improve and the Canterbury District Health Board had showed higher uptake was possible with 60 per cent of its nurses and 75 per cent of its midwives immunised, which was ‘much closer’ to the levels needed to protect vulnerable patients (7).

Influencing factors for low influenza immunisation amongst health care workers
Vaccination rates worldwide remain low despite strong evidence that immunisation of health care workers (HCWs) against flu is effective in preventing the spread of disease, lowers mortality rates among patients8,9, and that influenza infections in hospital health care workers lead to nosocomial outbreaks (10).
One qualitative research study found that nurses who chose not to be vaccinated did so for reasons of personal health choice and/or the perceived risk of injury or illness to themselves. The nurses viewed vaccination as a personal health choice and not an evidence-based nursing intervention. Patient safety outcomes were also mentioned as a factor influencing their decision to decline vaccination (11).
In another study undertaken in Minnesota, during the 2009 pandemic influenza outbreak, found a significant difference in vaccine uptake between doctors and nurses with 85 per cent of doctors and 62 per cent of nurses being vaccinated. More doctors than nurses chose vaccination because they believed they could accurately estimate their risk of side effects, while others identified a need to meet their professional obligation to be vaccinated and felt an ethical obligation to follow public health authorities’ recommendations and laws mandating pandemic vaccination (12).
A strong sense of professional responsibility was the strongest predictive factor for vaccination in a Saudia Arabian research project, as was previous positive experiences of vaccination (13).
A literature review of global barriers to vaccination uptake revealed consistent emergent themes across the varied nations carrying out the research studies. Themes identified included: fears about vaccine side effects; doubts around vaccine safety, efficacy and benefits in both pandemic and seasonal influenza scenarios; not viewing influenza as a serious illness; fear of contracting influenza; and fears that the vaccine could cause other illnesses such as Guillain-Barre syndrome and even infertility (14,15,16, 17).
Though recommended by many, and mandated by some, flu vaccination rates among HCWs, even in pandemics, remain below optimal levels (12).
Addressing the fears around vaccination
The latest Seasonal Influenza Vaccine report issued in New Zealand by the Centre for Adverse Reactions Monitoring (CARM)(18) reveals the number of adverse events reported in recent years (see Table 1).

The most commonly reported events were injection site inflammation [45 reports], fever [24], arm pain [22], vomiting [20] and headache [20].
On reviewing these results, several conclusions can be drawn. It appears that the number of adverse events reported in contrast to the potentially large number of vaccine doses administered is in fact very small. In 2012, adverse events equated to just 0.02 per cent and none of these events were life threatening. Also, while the type of adverse event reported may dissuade individuals from seeking vaccination, because of the temporary inconvenience of symptoms experienced, the actual or perceived threat of adverse events in this instance appears scientifically unsubstantiated.
A limitation of the CARM data is that only those who report adverse events post- vaccination are included in the results. How many went unreported? The robustness of the CARM data may be enhanced by identifying actual numbers of vaccines administered and providing more detail on those who reported events – e.g. age, gender plus how, where and when they were vaccinated. This may help in identifying trends. It may also be interesting to identify how many individuals actually contracted influenza post-vaccination? There is anecdotal evidence to suggest that some people do experience varying degrees of influenza-type illness post-vaccination and while other factors may contribute to individuals becoming unwell, is this a factor that contributes to reduced uptake of vaccination?
A review of the literature found no evidence to support or substantiate influenza vaccination causing infertility. There was a small link between influenza vaccination and Guillain-Barre Syndrome identified in America in the 1970s but those vaccine components have long since been discontinued and therefore pose no current threat.

Raising influenza vaccination uptake rates
Research study findings have identified a number of recommendations to raise influenza immunisation rates globally among health care workers. These include: improving education around vaccine use for health care workers to dispel myths and raise awareness (21); using the past and present experiences of influenza events to improve pandemic awareness and vaccination programme management targeted specifically at health care workers (22); starting education campaigns much earlier in a pandemic; (23) ensuring health care workers have access to scientific literature; having trust in public health communications and messaging; receiving encouragement from loved ones, physicians and co-workers; having access to vaccine campaigns that emphasise benefits of vaccination and highlight positive cues to vaccination while addressing barriers to vaccine uptake (24); effectively managing media to enhance the scientific validity of vaccination and influenza events reporting (25); and making health care worker vaccination mandatory26.
Vaccination: personal choice, professional responsibility or mandatory expectation?
Making health care worker vaccination mandatory has proved effective in improving influenza immunisation rates. Where this has been implemented, however, this has been met with resistance and caused controversy and substantial discontent (27). Controversy and discontent were in conflict over freedom of choice versus the mandate to ‘do no harm’ and ‘act in patients’ best interests. Freedom of choice breaches have the potential to adversely impact on individuals’ decisions based on religious, medical, or philosophical beliefs. The WHO, while advocating strongly for high health care worker vaccination levels, also respect individuals’ rights to abstain from vaccination on religious or medical grounds.
The costs of low influenza vaccination uptake rates among health care workers.
There is evidence of increased incidences of nosocomial influenza infections in hospital and community health care environments where vaccination rates are low28. The highly infectious nature of influenza can result in decimated health care worker numbers very quickly, even within immunised environments. The costs associated with managing seasonal, epidemic and pandemic influenza events – such as hospitalisation of infected people and replacing ill staff – can be billions of dollars29. Costs not only impact on health spending budget and health care organisations but also on individuals who potentially lose wages if unable to work for lengthy periods because they are unwell. Most sick leave allocations are minimal and just one ill health event that stops you working for even a couple of weeks can use up this precious resource very quickly. The threat of financial hardship is very real. Many colleagues will continue to work while experiencing varying degrees of influenza-type symptoms because the threat of financial hardship often precludes staying away from work or because they believe their own immune system will fight the infection. Unfortunately this only aids the spread of infection to patients and colleagues alike. Organisational policies aimed at containing the spread of influenza by sending sick staff home early, at symptom onset, are often not implemented.
Minimising the costs through managing the risks
Being vigilant with basic hand hygiene practices and following a lifestyle that promotes optimal health and well being have a valuable part to play in minimising the potential spread of influenza. Some other interventions for implementation can include health promotion campaigns such as advising people if they are feeling unwell to stay at home until they are better; to if possible take advantage of influenza vaccination; and to ensure adequate food stocks, medicines and tissues are available should they need to stay home in cases of seasonal, epidemic or pandemic influenza30. On April 1 this year, PHARMAC (New Zealand’s pharmaceutical management agency) extended the eligibility criteria for people receiving free influenza vaccination in a bid to prevent and or minimise disease spread and adverse population impacts31. Organisations may also benefit from reviewing their policies on staff sick leave for people demonstrating flu-like symptoms so that these can be implemented more efficiently and minimise infection spread to patients and colleagues alike.
Conclusion
Research has identified that influenza vaccination albeit for seasonal, epidemic or pandemic containment appears to be a lower priority for health care workers globally, especially nurses. Decisions about vaccination appear to be influenced by and closely linked to personal, professional and ethical beliefs, values and knowledge, which can cause conflict and confusion for health care workers.
Research has also identified that low vaccination uptake rates among health care workers are often related to fear and are not scientifically substantiated. Common fears include: fear of contracting the illness, experiencing vaccine side effects and doubts about vaccine efficacy. Educating health care workers using relevant, evidence-based information presented in a timely and effective manner is one intervention recommended for improving influenza vaccination uptake rates. Recommending mandatory vaccination for all health care workers to improve immunisation rates has resulted in some conflict and resistance. Health care workers believe their human right to choose in this instance has been superseded by the organisational and professional expectations to do no harm and act in the patients’ best interests. The WHO respects individual’s rights to choose to decline vaccination on the grounds of religious or medical grounds. Maintaining optimal health and wellness, coupled with vigilance when implementing basic hand and other hygiene measures are also effective in minimising the spread of influenza.
Responsibility for managing influenzas effectively and efficiently is a challenge for everyone. The costs of failing to do so are significant for nurses, their clients, colleagues, employing organisations, communities, health funding, governments, and global health outcomes. The World Health Organisation has and continues to develop new initiatives aimed at containing and effectively guiding the management of influenza outbreaks globally. The need for ongoing robust discussions, decisions, and actions to effectively manage the constant threat of rapidly mutating influenza virus strains remains ever present as will the debate about the role of vaccination in assisting this.
A quote from Hippocrates in closing: “A wise man should consider that health is the greatest of human blessings and learn how by his own thought to derive benefits from his illnesses”(32).
About the author:
Noreen McLoughlin RN MA (Applied) Diploma Adult Education & Training is an independent health auditor, self-employed professional evelopment consultant for the last seven years, and a registered nurse for 30 years.
This article was peer reviewed by:
- Nicola Russell RN BN M.Phil (Nursing) primary health care nurse, Invercargill and board member of College of Nurses Aotearoa (NZ).
- Gillian Sim RN BHSc, MA(hons) nurse researcher and public health nurse, Southern District Health Board.
Acknowledgements
My thanks are extended to the following people for their assistance in helping me track down and access some relevant research information for this article: Theo Brandt, communications manager for Immunisation Advisory Centre, University of Auckland; Michelle Kapinga and Brenda Saunders of the National Influenza Specialist Interest Group; Dr Michael Tatley, the Director of CARM; and Cory Vessey, Ministry of Health immunisation advisor.
View PDF of this article (and related learning activity) here >>
REFERENCES
- WORLD HEALTH ORGANISATION (2012) Meeting of the Strategic Advisory Group of Experts on Immunisation April 2012, Conclusions and Recommendations. WER, 2012, 21, 87, 201-216
- CENTRES FOR DISEASE CONTROL AND PREVENTION (2013) http://www.cdc.gov/vaccines/vac-gen/immunity-types.htm Retrieved May 2013
- IMMUNISATION ADVISORY CENTRE Duration of Protection, Efficacy and Effectiveness http://www.immune.org.nz/category/tags/vaccine-duration retrieved May 2013
- CENTRES FOR DISEASE CONTROL AND PREVENTION (2013) http://www.cdc.gov/vaccines/vac-gen/immunity-types.htm Retrieved May 2013
- IMMUNISATION ADVISORY CENTRE (2013) Immunisation overview 2013 www.immune.org.nz Retrieved May 2013
- MINISTRY OF HEALTH Workforce Influenza Coverage Rates 2010-2012 (November 20 2012 update) http://www.health.govt.nz/our-work/preventative-health-wellness/immunisation/updates-immunisation Retrieved 20 May 2013
- JENNINGS L Call for more nurses to get ‘flu jabs, Nursing Review News Feed April 2 2013 (from NISG press release March 27)
- HAYWARD A, HARLING R, WETTEN S, JOHNSON,AM, MUNRO S, SMEDLEY J, MURAD S, AND WATSON J (2006) Effectiveness of an influenza vaccine programme for care home staff to prevent death, morbidity and health service use among residents: cluster randomised controlled trial. British Medical Journal. 2006 Dec, 333 7581, p1241 retrieved from the Cochrane library April 16 2012
- CARMAN W, ELDER A, WALLACE L, MCAULEY K, WALKER A, MURRAY G, AND STOTT D (2000). Effects of influenza vaccination of health care workers on mortality of elderly people in long term care: a randomised controlled trial. Lancet 2000 Jan, 355 9198, pp 93-97. Retrieved from the Cochrane library April 16 2012
- VOIVIN N, BARRET B, METZGER M AND VANHEMS P (2009). Hospital Acquired Influenza. Synthesis using the outbreak reports and interventions studies of nosocomial infection statement. Journal of Hospital Infections 2009, 71: 1-14
- RHUDY L, TUCKER S, OFSTEAD C AND POLAND G (2010) Personal choice or evidence-based nursing intervention: nurses’ decision-making about influenza vaccination. Worldviews Evidence Based Nursing 2010 Jun 1;7(2):111-20 Epub 2010 Mar
- HENRIKSEN HELLYER J, DEVRIES A, JENKINS S, LACKORE K, ZIEGENFUSS J, POLAND G, AND TILBERT J (2011) Attitudes and uptake of H1N1 vaccine among health care workers during the 2009 H1N1 Pandemic. Plos One, 2011;6(12) epub 2011 Dec 22.
- AL-TAWFIQ JA (2012) Willingness of health care workers of various nationalities to accept H1N1 (2009) pandemic influenza A vaccination. Ann Saudi Med, 2012 Jan-Feb:32(1):64-7
- AGUILAR-DIAZ FEDL C, JIMENEZ-CORONA M, PONCE-DE-LEON-ROSALES S (2011) Influenza vaccine and health care workers. Arch Med Res, 2011 Nov;42(8):652-7 Epub 2012 Jan 4.
- CHOR J, NGAI K, GOGGINS W, WONG M, WONG S, LEE N, LEUNG T, RAINER T, GRIFFITHS S, AND CHAN P (2009). Willingness of Hong Kong health care workers to accept pre-pandemic influenza vaccination at different WHO alert levels: two questionnaire surveys. British Medical Journal. Aug 2009. http://www.ncbi.nlm.nih.gov/pubmed/19706937 Retrieved May 2013
- ALKUWARI M, AZIZ N, NAZZAL Z, AND AL-NUAIMI S (2011) Pandemic Influenza A/H1N1 vaccination uptake among health care workers in Qatar: motivators and barriers. Vaccine 2011 Mar 3;29(11):2206-11
- BOHMER M, WALTER D, FALKENHORST G, MUTERS S, KRAUSE G, AND WICHMANN O (2012) Barriers to pandemic influenza vaccination and uptake of seasonal influenza vaccine in the post-pandemic season in Germany. BMC Public Health 2012 Oct 31,12:93.
- CARM (2012) Seasonal Influenza Vaccine Reports in 2012. Retrieved from www.medsafe.govt.nz May 2013
- World Health Organisation, Global Vaccine Safety Initiative http://www.who.org Retrieved May 2013
- World Health Organisation, Global Vaccine Safety Blueprint http://www.who.org Retrieved May 2013
- TORUN S, AND TORUN F (2010) Vaccination against pandemic influenza A/H1N1among health care workers and reasons for refusing vaccination in Istanbul in last pandemic phase. Vaccine 2010 Aug 9;28(35):5703-10 epub 2010 Jun 30
- WICKER S, RABENAU H, BIASH, GRONEBURG D, AND GOTTSCHALK R (2010) Influenza A (H1N1) 2009: Impact on Frankfurt in due consideration of health care and public health. J Occup. Med Toxicol, 2010 April 26;5:10
- SEALE H, KAUR R, WANG Q, YANG P, ZHANG Y, WANG X, LI X, ZHANG Z, AND MACINTYRE C (2011) Acceptance of a vaccine against pandemic influenza A (H1N1) virus amongst health care workers in Beijing, China. Vaccine 2011 Feb 11;29(8):16705-10
- PREMATUNGE C, CORACE K, MCCARTHY A, NAIR RC, PUGSLEY R, AND GARBER G (2012) Factors influencing pandemic influenza vaccination of health care workers-a systematic review. Vaccine, 2012 Jul 6;30 (32):4733-43
- PETOUSIS-HARRIS H, GOODYEAR-SMITH F, KAMESHWAR K, AND TURNER N (2012) Fact or Fallacy? Immunisation arguments in the print media. Australian and New Zealand Journal of Public Health 34(5), 2010 521-526
- HOLLMEYER H, HAYDEN F, MOUNTS A AND BUCHHOLZ U (2012) Interventions to increase influenza vaccination among health care workers in hospitals. Influenza and other respiratory viruses 2012. DOI: 10.111/irv.12002
- CHOR J, PADA S, STEPHENSON I, GOGGINS W, TAMBYAH PA & ET AL (2011) Seasonal influenza vaccination predicts pandemic H1N1 vaccination uptake among health care workers in three countries. Vaccine Oct 6:29(43) epub 2011 Jul 30.
- SALGADO C, FARR B, HALL K AND HAYDEN F (2002) Influenza in the acute hospital setting. Lancet Infectious Diseases 2002; 2:145-155
- DOHERTY P Vets and viruses (2013) Radio Broadcast with Kim Hill, Radio NZ National, Saturday May 18 2013.
- Ministry of Health (2013) Influenza www.health.govt.nz/your-health/conditions-and-treatments/diseases-and-illnesses Retrieved May 2013
- PHARMAC (Pharmaceutical Management Agency) (2013) Amendment to Influenza Vaccine Funding Criteria
- Hippocrates www.brainyquotes.com
This learning activity is relevant to the Nursing Council competencies related to leading and participating in quality improvement activities for RNs, ENs and NPs.
Learning Objectives
Reading and reflecting on this article will enable you to:
- Outline elements and stages in planned organisational change.
- Identify ways that resistance to change can be understood positively.
- Think about your own role and competence in relation to change management.
Introduction
Change management is a fundamental element in quality and improvement processes. It is also at the heart of leadership. Those implementing change need first to disrupt the status quo, secondly, to move everyone and everything involved to a new way of doing things, and finally, to ensure that the new practice and processes cannot change back to the former state. Change leaders are advised to do everything possible to predict and manage resistance to the proposed change. Ironically, suppressing resistance – rather than actively encouraging concerns and critiques to surface – compromises not only acceptance of the change process but also its robustness and sustainability. In this learning activity, we’ll revisit Lewin’s classic theory of planned change in the light of new thinking about resistance and readiness.
Change and stability in the health system
Articles on organisational change in health services often open with statements about the inevitability, increasing pace, and necessity of change – perhaps making change-weary readers feel even more weary. But what doesn’t change? The need for health services and health professionals’ willingness to provide them are two things that endure (6). Health care systems such New Zealand’s, or the National Health Service in the United Kingdom, have been subjected to large scale ‘redisorganisations’ (7) bringing about significant (and enduring) changes in health service structures, funding, and accountability. Yet, through all this, it can be argued that health professionals have retained significant control at a micro or clinical level (4,8).
The clinical level presents both the most potential to make real improvements in care, and, because any change must be negotiated within and between teams (which in turn, are part of interrelated systems), the most difficulty (9). Lewin’s work on planned change, tested in difficult social change projects, is relevant and helpful because it is based on the group – defined not on the basis of similarity or dissimilarity of individuals but their interdependence (10).
Box 1: What drives organisational change
Organisations change to anticipate, adapt, or respond to change in their environments or to find ways to better fulfill their mission.
Revolutionary change (also referred to as strategic, radical, fundamental, ‘big-bang’, transformational change) involves sharp and simultaneous shifts across many organisational dimensions – structure, strategy, ideology, power relations, cultural systems of meaning, and control mechanisms. It is often thought to be driven by external political or market forces or other threats to the organisation’s viability, but internally, pressure to change and the capacity to take action is also necessary.
Evolutionary, incremental or convergent change fine-tunes an organisation without abandoning its basic structures and systems, nor the framework of shared interpretations and understandings held by organisation members.
Whether organisational change is considered revolutionary or evolutionary depends on the pace and scale of adjustment and upheaval: revolutionary change affects all parts of the organisation and happens relatively quickly; evolutionary change may happen differently in different parts of the organisation and happens relatively slowly and gradually. New technologies may be the driver or enabler in either scenario (1,2,3,4,5).
Goals for health service change
Change without a clearly identified causative reason can be viewed as ‘change for change’s sake’. But aims for innovation and improvement in health care identified in the United States11 present clear, compelling, and enduring goals for all health systems (12). By the acronym S-T-E-E-E-P, they are:
- Safety – reducing treatment related injuries and harm to patients
- Timeliness – reducing waits and delays throughout the health system
- Effectiveness – increasing the reliability of care through an evidence base
- Efficiency – reducing the total cost of care
- Equity – reducing disparities in health outcomes
- Patient centredness – giving patients and carers far more voice, control, and competence in self-management (11,12).
Change competencies
These goals certainly represent a challenge when contrasted with the need to competently manage change. This need is highlighted by reports that estimate:
- up to 70% of change initiatives do not succeed (13)
- the rate of quality improvement implementation in healthcare is less than 50% (14)
- translation of research findings into routine clinical practice may be delayed up to two decades (15).
Effective change implementation and building sustained change capability are emerging as general leadership requisites, but these are especially needed in complex organisations such as health services (5,13). Whether those involved in innovation or improvement processes see themselves as change managers, change leaders, or change agents, they need to be able to:
- Create the case for change by effectively engaging others in recognising the business need for change.
- Create structural change by ensuring that the change is based on depth of understanding of the issues and supported with a consistent set of tools and processes.
- Engage others in the whole change process and building commitment.
- Implement and sustain changes by developing effective plans and ensuring good monitoring and review practices are developed.
- Facilitate and develop capability by ensuring that people are challenged to find their own answers and that they are supported in doing this (13).
Managing change: Resistance and readiness
Resistance
… no business survives over the long term if it can’t reinvent itself. But, human nature being what it is, fundamental change is often resisted mightily by the people it most affects: those in the trenches of the business. Thus, leading change is both absolutely essential and incredibly difficult (19).
Resistance to change has been described as any conduct that has the effect of maintaining the status quo in the face of pressure to alter it, and is often linked with negative attitudes and undermining behaviour (20). Even small scale incremental change designed to make a real difference in quality and safety of care for patients – at the front line – can find the would-be change agent feeling apprehensive about being taken out by ‘friendly fire’.
However, defensive or adversarial approaches designed to pre-empt resistance can provoke objections that weren’t there in the first place (20).
The idea that little or no resistance is the sign of a successful change project is being challenged in arguments for the utility of resistance. Most compelling is the idea that resistance contributes to robustness in the change process:
- proposals that are not properly thought through, inappropriate, or just ‘plain wrong’ are questioned
- more alternatives are generated and evaluated, from more perspectives, allowing the possibility of synthesizing different opinions and expertise (20).
Moreover, resistance to change can be seen as a legitimate and human response (20) that is:
- preferable to acquiescence or apathy – which also threaten the likelihood of the change being implemented;
- often about the uncertainties and potential outcomes of a proposed change (rather than the change itself), especially as they impact on the individual or disrupt notions of equity within a team or between roles (1,2);
- to be expected if change feels imposed or there is a noticeable discrepancy between espoused values and what actually happens (2,6).
Readiness
[Good leaders] help people see and articulate what [is] wrong… make them intrinsically unhappy with the current state of affairs without demeaning their accomplishments or dishonouring their past in any way (21).
Accompanying a rethinking of resistance is new thinking on how to prepare for change more positively. This is an important consideration when change projects in health services are often prompted by some sort of failure or negative – perhaps audit results are not as they should be or a patient has been harmed in an adverse event. (An alternative approach to change, based on understanding what we do well, is appreciative inquiry (22,23,24)).
Armenakis and his colleagues (1) recommend that change managers communicate a consistent change message to convey the nature and meaning of the change, helping shape staff perceptions and responses. Their three stage change model (readiness – adoption – institutionalisation) incorporates social learning theory, which proposes that most behaviour is learned through observation and modelling (25).
According to Armenakis et al an effective change message has five elements:
- Discrepancy ‘We know we need to change’
- Appropriateness ‘We have agreed this is the right change to make’
- Efficacy ‘We can cope with change and we have the capability to change successfully’
- Principal support ‘Those the change affects are behind it, and it has the support it needs’
- Personal valence ‘It is in my best interest to change’ (1)
For this message to be credible, it must be congruent with experience – the staff feel they have been involved and consulted, they have the skills, and they can see what it will mean for their practice.
What is your position?
If leadership is a social influence process, in which connectedness between the leader and the individual is the most powerful component (26), where in the organisation should commitment, capability, and competencies for leading change be positioned?
Executive level leadership – ‘from the top’ – is critical in strategic or fundamental change which involves the culture or identity of the organisation. However, there are arguments that – especially in large and complex health service organisations – ‘distant’ executive leaders (while actively supporting innovation and improvement) cannot do what ‘close’ or ‘nearby’ first-line and middle managers are well positioned to do, which is having the ongoing conversations that facilitate understanding and learning at the clinical level (12,13,26). Those with change agent roles (for example, leading an improvement project) may not have the positional power of line management, but their expertise and ability to work with people gives them credibility (27).
These roles (your role perhaps) integrate organisational strategy with operations and bridge management and professional cultures (8). Critically, it is at the team level that leaders can build a supportive social climate that buffers the agitating and distracting effects of any uncertainty for the wider organisation (28). They can help staff make sense of a change process by telling the change message consistently. One study found managers simultaneously using ‘progressive narratives’ about the ‘what’, ‘how’, and ‘why’ of change, along with ‘stability narratives’, which preserved existing messages about the organisation’s purpose (29). Being close to the work, they have an immediate and continuous influence over the mundane but critical business of changing habits and routines (30).
In ‘nearby’ leadership roles it is possible to see what practical steps should be taken to support the skill development required, and to make it happen. An example is a study of a challenging technology adoption (cardiac surgery) where the successful teams had carefully selected their members, ran practice sessions (which created psychological safety and helped develop a shared mental model of the new procedure), and reviewed their learning to create further improvement (3).
Leadership near the front line is well placed to recognise the pressures on individuals to work harder and deliver continuous improvements in performance (13), and therefore, to advocate for autonomy, realistic expectations and resources for specific change efforts, and building change capability within the team (28).
Following Lewin’s belief that learning is the process that enables individuals to understand and restructure their perceptions of the world around them10, change leaders can reframe change itself as a process of managed learning (3,16), and learning as an enabler of change that empowers and transforms individuals and teams in their work (31).
Looking at it this way, is the managing of meaning in change a role you can take?
Box 2: Lewin’s Planned Change Theory
Kurt Lewin (1890-1947), recognised by his contemporaries as an innovative and influential social scientist, is mainly remembered today for just one part of his Planned Change theory – the 3 Step Model (10).
His deep commitment to democratic values caused him first to flee Nazi Germany for America and then informed a programme of research encompassing diverse aspects of social conflict, including problems experienced by minority and disadvantaged groups.
The result of Lewin’s theory development and humanitarian research was an approach to Planned Change. It integrates four elements designed to be taken as a whole:
- Field Theory and Group Dynamics, which explain how groups are formed, motivated, and maintained, and
- two methods to change group behaviour, Action Research and the 3 Step Model.
Critics of the 3 Step Model as outdated or simplistic have been referred to this larger conceptual framework as providing answers to their points (10), and it’s worth highlighting that the model focuses on changing group perceptions and behaviour (because individuals conform to group pressures) rather than concentrating on individual behaviour.
Schein uses Lewin’s own famous dictum, ‘There is nothing so practical as a good theory’, to commend the 3 Step Model as a framework for understanding human change as a profound psychological process involving painful unlearning and difficult relearning (16).
Transition through stages of change described in the 3 Step Model is evident in many models of change.
Box 3: 3 Step Model for a planned change process
Unfreezing: Motivation to change comes from accepting that the current situation is not satisfactory, a desire or sense of obligation to address what is not right, and critically, so that people don’t take defensive positions or deny the existence of a problem, a safe psychological environment (16). Information or insights that challenge the validity of the status quo may come from quality monitoring and benchmarking, patient complaints, or consumer consultation, investigation of adverse events or near misses, or staff speaking up about obstacles, errors, or opportunities for improvement (17). Unfreezing reduces resistance and helps readiness for change.
Moving: Implementing the solutions identified as most appropriate (in a participative and collaborative action research process) also requires destabilising the equilibrium between the forces ‘driving’ and ‘restraining’ the group. For example, lack of knowledge and skills acts as a restraining force, but implementing training for staff to develop new skills required in changed practice becomes a driving force. Simply increasing the expectation of changed performance, without decreasing the difficulty of making the changes, means ‘higher aggressiveness, higher emotionality, and lower constructiveness’ (18).
Refreezing: Without new norms, policies, and practices to act as forces holding group attitudes and behaviour in a new equilibrium – and congruent with what the group values – performance may drift back to return to its earlier state. The new way of doing things must be reinforced, aligned with other organisational procedures and routines, and thus, institutionalised (2,10). For instance, making the new behaviour count helps it to stick: ‘What gets measured gets done, what gets rewarded gets done repeatedly’.
QUESTIONS THIS ARTICLE MIGHT PROMPT YOU TO ASK YOURSELF
- How might Lewin’s 3 Step Model be useful in the next change process I am involved with?
- Do I resist change processes at work? What are my reasons?
- Is there a change process I know of that went well? What helped people be ready?
View PDF of this article (and related learning activity) here >>
Recommended reading and resources
Articles
- WADDELL D & SOHAL AS (1998) Resistance: A constructive tool for change management. Management Decision 36(8):543–548.
- EDMONDSON AC, BOHMER RM & PISANO GP (2001) Disrupted routines: Team learning and new technology implementation in hospitals. Administrative Science Quarterly 46(4):685-716.
Web resources
- Published in Harvard Business Review in 1995, Kotter’s classic short article, Leading Change: Why Transformation Efforts Fail is available here: https://cb.hbsp.harvard.edu/resources/marketing/docs/95204f2.pdf
- At the United States based Institute for Healthcare Improvement, sign in (free) to the online IHI knowledge centre to access the ‘Changes for Improvement’ resource page www.ihi.org/knowledge/Pages/Changes/default.aspx where you can download a white paper: REINERTSEN JL, BISOGNANO M, PUGH MD (2008) Seven Leadership Leverage Points for Organisation-Level Improvement in Health Care (Second Edition). Cambridge, Massachusetts: Institute for Healthcare Improvement; 2008.
- On this webpage you will find a useful set of short articles by Helen Bevan, Chief of Service Transformation at the NHS Institute for Innovation and Improvement: http://www.ihi.org/resources/Pages/AudioandVideo/ProfilesinImprovementHelenBevanNHSIII.aspx
- It’s worth exploring short courses in massive open online courses (MOOCs). For instance, at the Stanford led www.coursera.org/ relevant topics include leading strategic innovation in organisations, healthcare innovation and entrepreneurship, and organisational analysis.
About the author:
Shelley Jones RN BA MPhil has been working in nursing professional development for 30 years.
Acknowledgements:
Thank you to peer reviewers Sam Denny and Faith Roberts for their helpful critique.
REFERENCES:
- ARMENAKIS AA & BEDEIAN AG (1999) Organisational change: A review of theory and research in the 1990s Journal of Management 25(3):293-315.
- BOYETT J & K (1998) The Guru Guide: The Best Ideas of the Top Management Thinkers. Chapter 2 ‘Managing Change’. John Wiley: New York NY.
- EDMONDSON AC, BOHMER RM & PISANO GP (2001) Disrupted routines: Team learning and new technology implementation in hospitals. Administrative Science Quarterly 46(4):685-716.
- McNULTY T & FERLIE E (2004) Process transformation: Limitations to radical organisational change within public service organisations. Organisation Studies 25(8):1389-1412.
- YUKL G, GORDON A & TABER T (2002) A hierarchical taxonomy of leadership behavior: Integrating a half century of behavior research. Journal of Leadership and Organisation Studies 9(1):15-32.
- I am grateful to have heard Professor George Salmond, public health physician and champion, former Director-General of Health, make a compelling argument (in a comment from the floor) that partnership between consumers and health professionals represents an alliance that endures through periodic political and structural reorganisations of health services.
- OXMAN AD, SACKETT DL, CHALMERS I & PRESCOTT TE (2005) A surrealistic mega-analysis of redisorganisation theories. Journal of the Royal Society of Medicine 98:563–568.
- JONES SER (1994) Career Transition: From Professional to Manager in the Health Service. (Unpublished master’s thesis). University of Auckland, New Zealand.
- KOECK C (1998) Time for organisational development in healthcare organisations: Improving quality for patients means changing the organisation. British Medical Journal 317:1267–8.
- BURNES B (2004) Kurt Lewin and the planned approach to change: A re-appraisal. Journal of Management Studies 41(6):977-1002.
- INSTITUTE OF MEDICINE (2001) Crossing the Quality Chasm: A New Health System for the 21st Century. National Academy Press: Washington, DC.
- BERWICK DM (2004) The improvement horse race: Bet on the UK. Quality and Safety in Health Care 13:407-409.
- HIGGS M (2003) How can we make sense of leadership in the 21st century? Leadership & Organisation Development Journal 24(5):273-284.
- BIRKEN SA, LEE SD & WEINER BJ (2012) Uncovering middle managers’ role in healthcare innovation implementation. Implementation Science 2012, 7:28.
- GRAHAM ID, LOGAN JH, HARRISON MB et al (2006) Lost in knowledge translation: Time for a map? Journal of Continuing Education in the Health Professions 26(1):13-24.
- SCHEIN E H (1996) Kurt Lewin’s change theory in the field and in the classroom: notes towards a model of management learning. Systems Practice 9(1): 27-47.
- WEST E (2000) Organisational sources of safety and danger: Sociological contributions to the study of adverse events. Quality in Health Care 9:120-126.
- LEWIN K (1947/1999) Group decision and social change. In GOLD M (Ed), The Complete Social Scientist: A Kurt Lewin Reader (pp 265-284). American Psychological Association: Washington.
- Editor’s note in 2007 reprint of KOTTER JP (1995) Leading change: Why transformation efforts fail. Harvard Business Review.
- WADDELL D & SOHAL AS (1998) Resistance: A constructive tool for change management. Management Decision 36(8):543–548.
- NAYAR V (2010) Employees First, Customers Second. Turning Conventional Management Upside Down. Harvard Business Press: Boston MA.
- COOPERRIDER DL & SRIVASTVA S (1987) Appreciative inquiry in organisational life. Research in Organisational Change and Development 1:129-169.
- BROOKES J (2011) Engaging staff in the change process. Nursing Management 18(5):16-19.
- MOODY RC, HORTON-DEUTSCH S & PESUT DJ (2007) Appreciative inquiry for leading in complex systems: Supporting the transformation of academic nursing culture. Educational Innovations 46(7):319-324.
- INSTRUCTIONAL DESIGN (nd) BANDURA Social Learning Theory (A. Bandura). Retrieved from www.instructionaldesign.org/theories/social-learning.html
- ALIMO-METCALFE B & ALBAN-METCALFE J (2005) Leadership: Time for a new direction? Leadership 1(1): 51-71.
- McGILL ME & SLOCUM JW (1998) A little leadership, please? Organisational Dynamics 26(3):39-49.
- McDERMOTT AM & KEATING MA (2012) Making service improvement happen: The importance of social context. Journal of Applied Behavioral Science 48(1):62-92.
- SONENSHEIN S (2010) We’re changing – or are we? Untangling the role of progressive, regressive, and stability narratives during strategic change implementation. Academy of Management Journal 53(3):477-512.
- RERUP C & FELDMAN MS (2011) Routines as a source of organizational schema: The role of trial-and-error learning. Academy of Management Journal 54(3):577-610.
- LIEDTKA J (1999) Linking competitive advantage with communities of practice. Journal of Management Inquiry 8(1):5-16.